Final ID: Mo3009
Lesion Synergy or a Danger Zone? - Myocardial Perforation After Successive, Co-localized Pulse Field and Radiofrequency Ablations For Atrial Arrhythmia - Report of Two Cases and Discussion of Potential Mechanisms
Abstract Body (Do not enter title and authors here):
Introduction:
Pulsed Field Ablation (PFA) is becoming popular for Atrial Fibrillation (AF) ablation due to its improved safety profile. However, there are situations where a combination of PFA and Radiofrequency Ablation (RFA) may be indicated. We herein report two cases where PFA was followed by RFA, resulting in cardiac perforation.
Case #1:
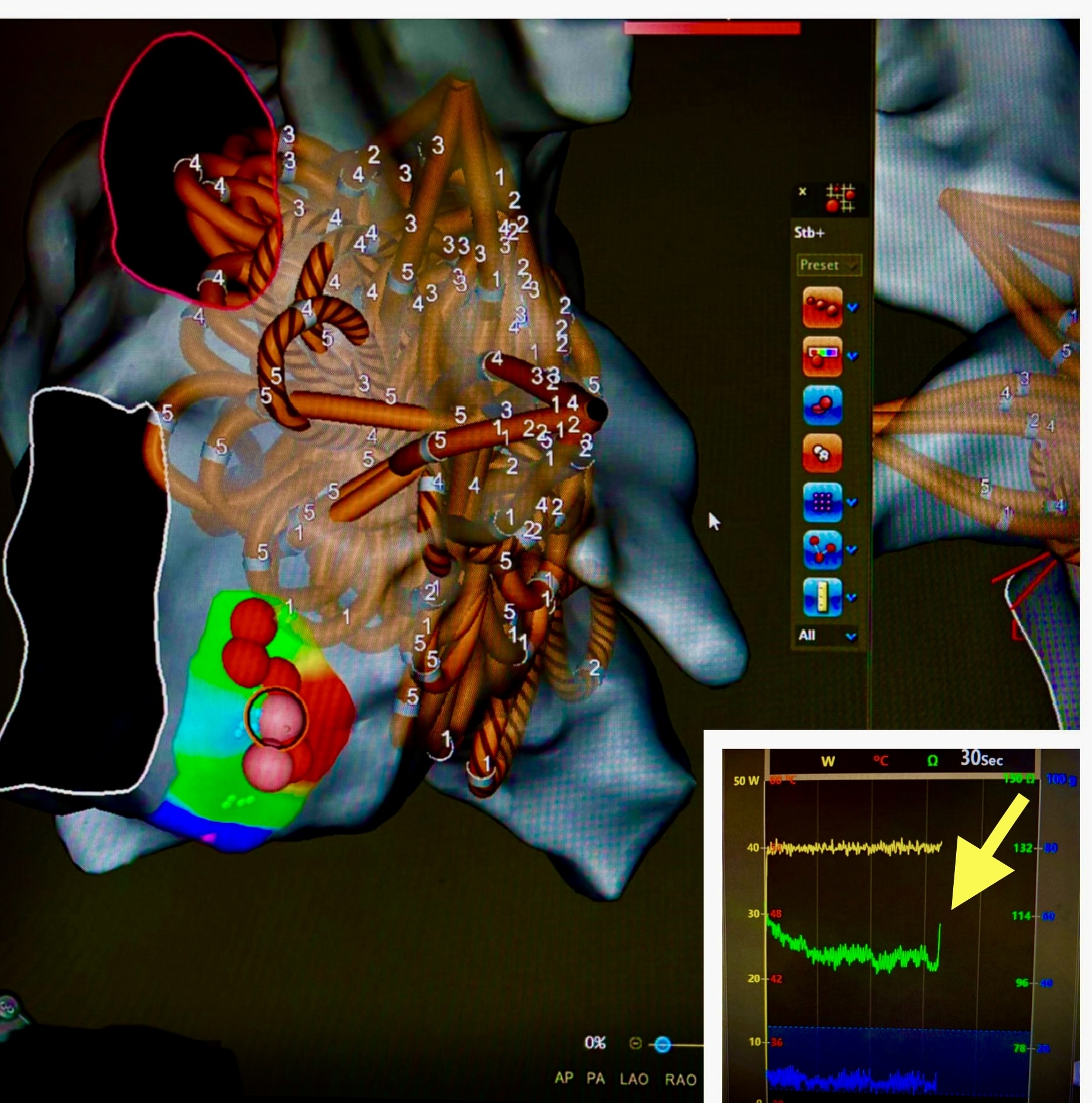
A 36-year-old male underwent catheter ablation (CA) for a highly symptomatic AF and supraventricular tachycardia. A concealed Left Lateral Accessory Pathway (LLAP) was diagnosed. Because of incessant degeneration to AF during the study, ablation of AF was undertaken first with wide area Pulmonary Vein Isolation (PVI) and Posterior Wall Ablation (PWA) using PFA. Subsequently, the LLAP was ablated using RFA. Suddenly, an acute impedance rise was noted (Image 1). The patient became hemodynamically unstable and had a large pericardial effusion.
Case #2:
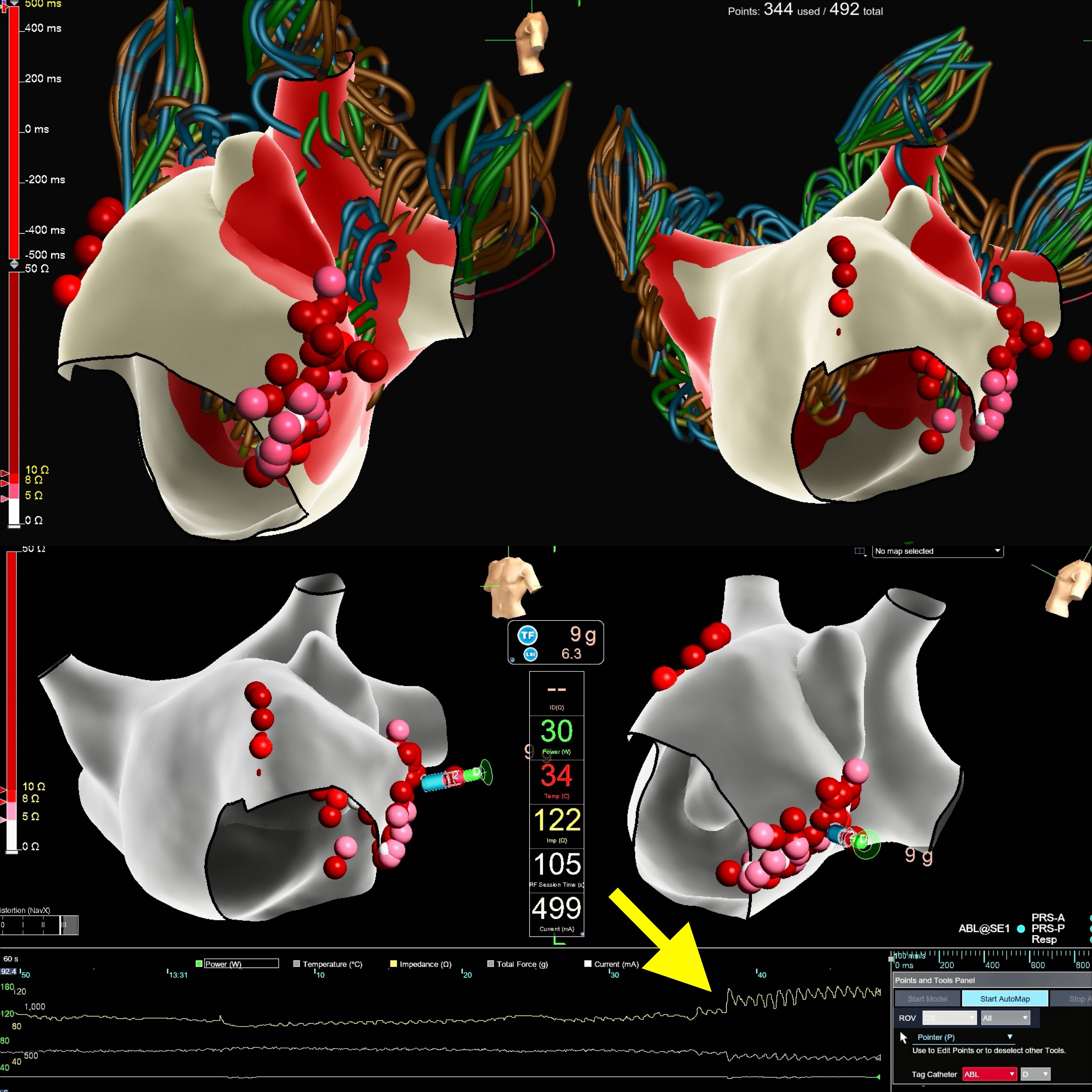
A 72-year-old male was referred for CA of AF. After PVI and PWA with PFA, refractory atrial flutter developed due to mitral annular flutter. To avoid giving high-dose nitroglycerin (NTG) to prevent coronary spasm in PFA, RFA was used to create a linear lesion from the left inferior PV down to the mitral valve. During RFA, an impedance spike was noted (Image 2). The patient’s blood pressure dropped, and Intracardiac echo revealed a large pericardial effusion.
Discussion:
PFA creates myocardial lesions with minimal thermal effects and has properties of myocardial tissue specificity as compared to RFA.
However, there may be situations where RFA is desired as well; for our first case, we wished to use a focal RF catheter to ablate an accessory pathway; in the second case, RF was chosen to avoid PFA on the mitral annulus that would have required high-dose prophylactic NTG administration. PFA changes tissue characteristics, and it can create larger lesions with subsequent RFA. Although this synergistic effect may be quite useful, especially in the ventricles where larger/deeper lesions may be desired, it may also be fraught with a higher risk of cardiac perforation.
It is of interest that both cases reported here involved RFA on the mitral annulus subsequent to PFA lesions delivered for PVI. However, it remains unclear how close in proximity to PFA lesions RFA lesions need to be delivered to produce a synergistic effect.
Conclusion:
Based on the discussion above, caution is warranted when using both forms of energy during catheter ablation of atrial arrhythmias.
Introduction:
Pulsed Field Ablation (PFA) is becoming popular for Atrial Fibrillation (AF) ablation due to its improved safety profile. However, there are situations where a combination of PFA and Radiofrequency Ablation (RFA) may be indicated. We herein report two cases where PFA was followed by RFA, resulting in cardiac perforation.
Case #1:
A 36-year-old male underwent catheter ablation (CA) for a highly symptomatic AF and supraventricular tachycardia. A concealed Left Lateral Accessory Pathway (LLAP) was diagnosed. Because of incessant degeneration to AF during the study, ablation of AF was undertaken first with wide area Pulmonary Vein Isolation (PVI) and Posterior Wall Ablation (PWA) using PFA. Subsequently, the LLAP was ablated using RFA. Suddenly, an acute impedance rise was noted (Image 1). The patient became hemodynamically unstable and had a large pericardial effusion.
Case #2:
A 72-year-old male was referred for CA of AF. After PVI and PWA with PFA, refractory atrial flutter developed due to mitral annular flutter. To avoid giving high-dose nitroglycerin (NTG) to prevent coronary spasm in PFA, RFA was used to create a linear lesion from the left inferior PV down to the mitral valve. During RFA, an impedance spike was noted (Image 2). The patient’s blood pressure dropped, and Intracardiac echo revealed a large pericardial effusion.
Discussion:
PFA creates myocardial lesions with minimal thermal effects and has properties of myocardial tissue specificity as compared to RFA.
However, there may be situations where RFA is desired as well; for our first case, we wished to use a focal RF catheter to ablate an accessory pathway; in the second case, RF was chosen to avoid PFA on the mitral annulus that would have required high-dose prophylactic NTG administration. PFA changes tissue characteristics, and it can create larger lesions with subsequent RFA. Although this synergistic effect may be quite useful, especially in the ventricles where larger/deeper lesions may be desired, it may also be fraught with a higher risk of cardiac perforation.
It is of interest that both cases reported here involved RFA on the mitral annulus subsequent to PFA lesions delivered for PVI. However, it remains unclear how close in proximity to PFA lesions RFA lesions need to be delivered to produce a synergistic effect.
Conclusion:
Based on the discussion above, caution is warranted when using both forms of energy during catheter ablation of atrial arrhythmias.
More abstracts on this topic:
Abl1 kinase-deficient mouse hearts exhibit conduction disturbance and arrhythmia vulnerability to oxidative stress that are typically associated with age-related proarrhythmic remodeling
Choi Bum-rak, Bronk Peter, Li Xiaofei, Song Yi, Kim Tae Yun, Lu Yichun, Radice Glenn
Adverse Events with Pulsed Field Ablation - A Review of the Food and Drug Administration’s Manufacturer and User Facility Device Experience DatabaseCooper Julie, Zagrodzky William, Zagrodzky Jason, Omotoye Samuel, Sardana Mayank, Kaplan Andrew, Link Mark, Bunch Thomas, Daniels James