Final ID: MP62
Hemodynamic Effects of Guideline-Based Sedation in Mechanically Ventilated Adults: A Multi-center Observational Analysis
Abstract Body (Do not enter title and authors here): Background: Propofol is a first-line sedative for critically ill adults receiving invasive mechanical ventilation (IMV). However, it can contribute to hemodynamic instability, especially in the setting of intubation. The magnitude, timing, risk factors, and variability of sedation-associated mean arterial pressure (MAP) changes remain poorly characterized in ICU settings.
Objectives: To quantify MAP changes following propofol sedation, identify risk factors for hemodynamic instability, and characterize associated interventions.
Methods: We included adults (≥18 years old) across 11 ICUs in the Mayo Clinic Enterprise who required IMV and received ≥6 consecutive hours of propofol infusion between 05/05/2018 and 07/31/2024. The primary outcome was MAP change within 2-hours following sedation. Secondary outcomes included vasopressor use and hypotension (MAP ≤60 mmHg). Mixed-effects modeling was utilized to account for individual patient differences. The main model used a “neutral” adjustment, estimating a 5 mmHg MAP increase per 0.05 mcg/kg/min of norepinephrine equivalents, reduced to 3 mmHg per 0.05 mcg/kg/min after reaching a dose of 0.20 mcg/kg/min. Those on any vasopressors prior to propofol sedation initiation were analyzed separately.
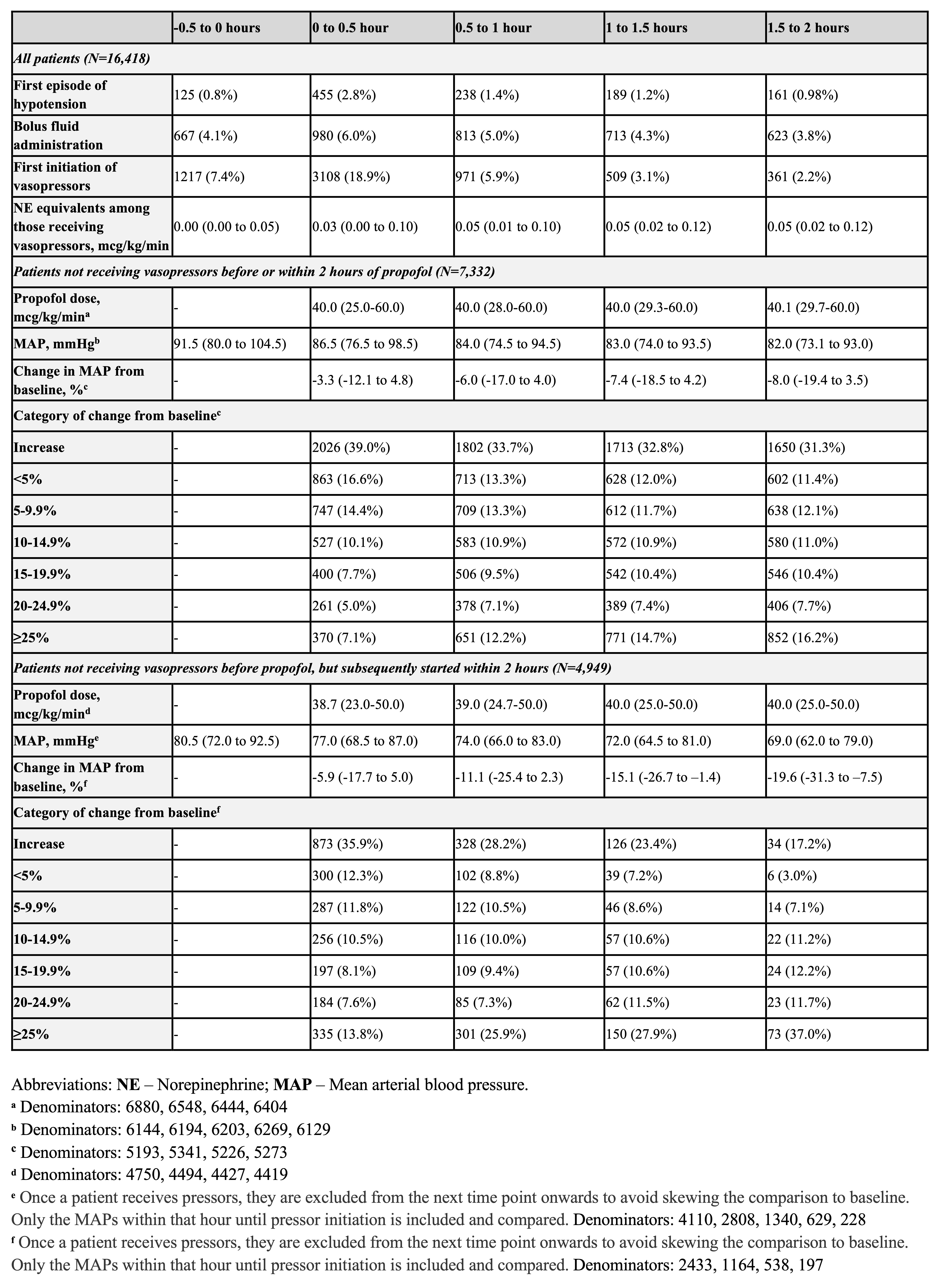
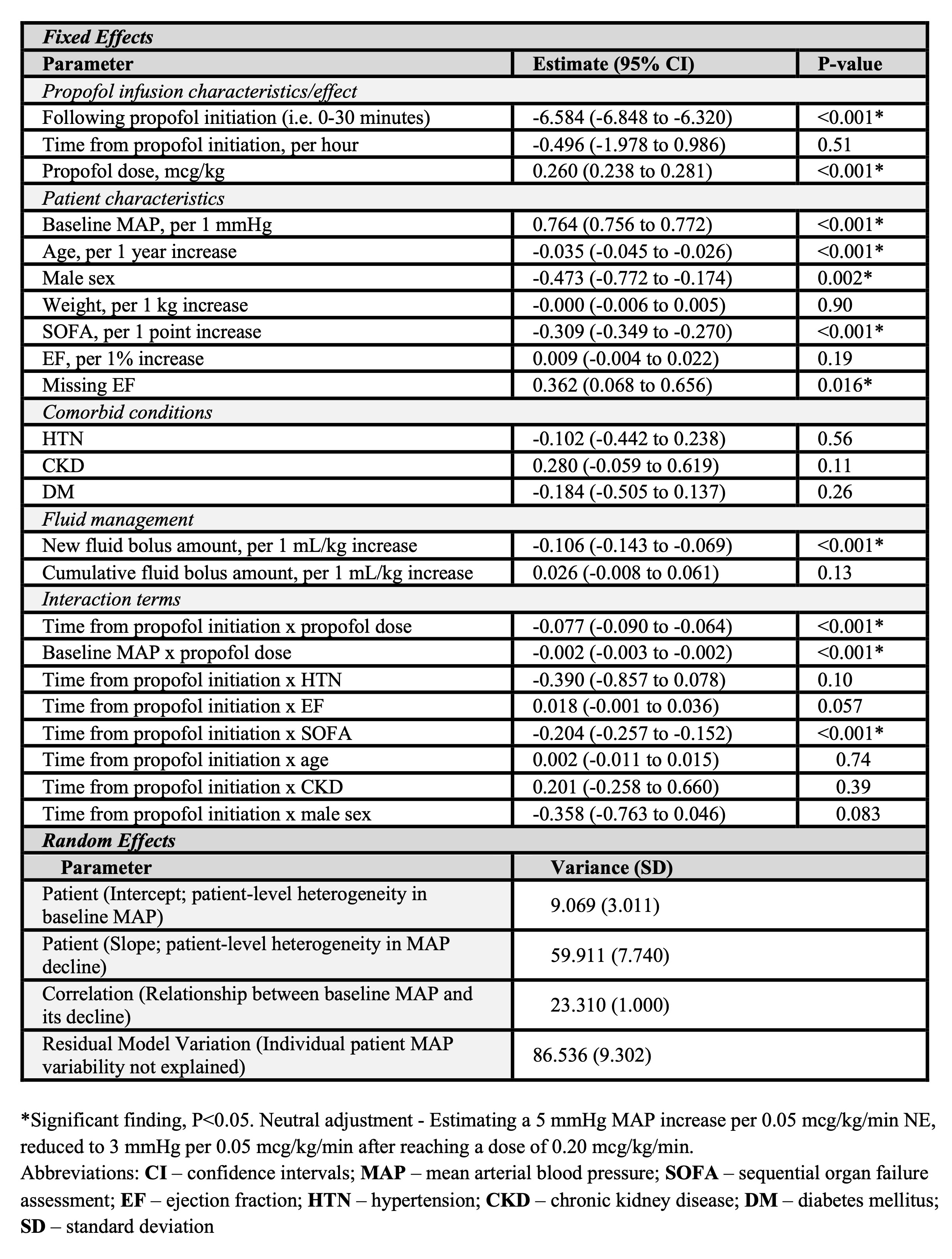
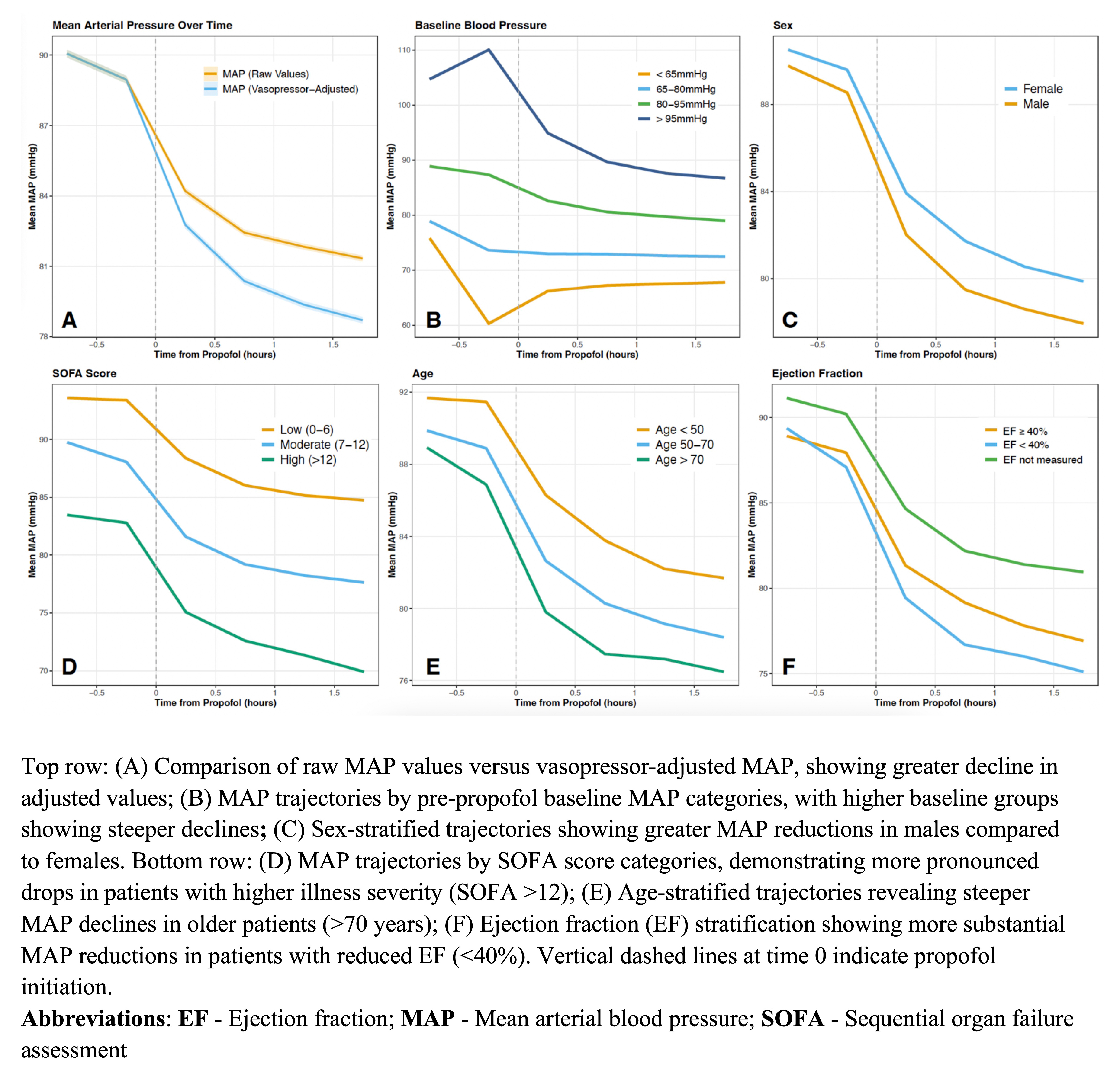
Results: Across 16,418 patients, 25.2% were on vasopressors before sedation initiation. Among the remaining 12,281 patients, 40.3% required vasopressors and 7.7% experienced hypotension within 2 hours of sedation (Image 1). Post-intubation sedation was associated with a MAP reduction within the first 30 minutes (-6.58 mmHg; 95% CI: -6.85 to -6.32; P<0.001; Images 2 and 3). There was substantial inter-patient variability in both baseline MAP (9.5% variation attributable to between-patient differences) and MAP decline after sedation (40.9% between-patient differences). Higher SOFA scores (-0.31 mmHg per point), older age (-0.04 mmHg per year), and male sex (-0.47 mmHg) were associated with lower MAP. Patients with higher illness severity experienced progressively greater MAP changes over time (-0.20 mmHg per hour per increasing SOFA point; P<0.001).
Conclusions: Propofol sedation is associated with clinically significant hemodynamic effects requiring intervention in the early post-intubation period. The marked inter-patient variability in hemodynamic responses highlights the importance of personalized management approaches. Risk stratification may help identify patients who could benefit from preemptive hemodynamic optimization.
Objectives: To quantify MAP changes following propofol sedation, identify risk factors for hemodynamic instability, and characterize associated interventions.
Methods: We included adults (≥18 years old) across 11 ICUs in the Mayo Clinic Enterprise who required IMV and received ≥6 consecutive hours of propofol infusion between 05/05/2018 and 07/31/2024. The primary outcome was MAP change within 2-hours following sedation. Secondary outcomes included vasopressor use and hypotension (MAP ≤60 mmHg). Mixed-effects modeling was utilized to account for individual patient differences. The main model used a “neutral” adjustment, estimating a 5 mmHg MAP increase per 0.05 mcg/kg/min of norepinephrine equivalents, reduced to 3 mmHg per 0.05 mcg/kg/min after reaching a dose of 0.20 mcg/kg/min. Those on any vasopressors prior to propofol sedation initiation were analyzed separately.
Results: Across 16,418 patients, 25.2% were on vasopressors before sedation initiation. Among the remaining 12,281 patients, 40.3% required vasopressors and 7.7% experienced hypotension within 2 hours of sedation (Image 1). Post-intubation sedation was associated with a MAP reduction within the first 30 minutes (-6.58 mmHg; 95% CI: -6.85 to -6.32; P<0.001; Images 2 and 3). There was substantial inter-patient variability in both baseline MAP (9.5% variation attributable to between-patient differences) and MAP decline after sedation (40.9% between-patient differences). Higher SOFA scores (-0.31 mmHg per point), older age (-0.04 mmHg per year), and male sex (-0.47 mmHg) were associated with lower MAP. Patients with higher illness severity experienced progressively greater MAP changes over time (-0.20 mmHg per hour per increasing SOFA point; P<0.001).
Conclusions: Propofol sedation is associated with clinically significant hemodynamic effects requiring intervention in the early post-intubation period. The marked inter-patient variability in hemodynamic responses highlights the importance of personalized management approaches. Risk stratification may help identify patients who could benefit from preemptive hemodynamic optimization.
More abstracts on this topic:
Comparison of Manual Versus Mechanical Ventilation During Cardiopulmonary Resuscitation in Pediatric Swine
Lapid Francis, Javdan Cameron, Maimie Kpehe, Lage Larraine, Obrien Caitlin, Shaffner Donald
Development of Bioimpedance for the Measurement of Ventilation During Cardiopulmonary ResuscitationPrakash Rithika, Jarrett Philip, Idris Ahamed