Final ID: MP900
Impact of Surgical Selection on Stroke and Survival in Aortic Arch Aneurysm: A Risk-Adjusted Comparison Between Total Arch Replacement and Thoracic Endovascular Aortic Repair Using Najuta
Abstract Body (Do not enter title and authors here): Objective: The aim of this study was to compare clinical outcomes between total arch replacement (TAR) and thoracic endovascular aortic repair (TEVAR) using Najuta in patients with aortic arch aneurysms, based on individual risk profiles including frailty and surgical risk.
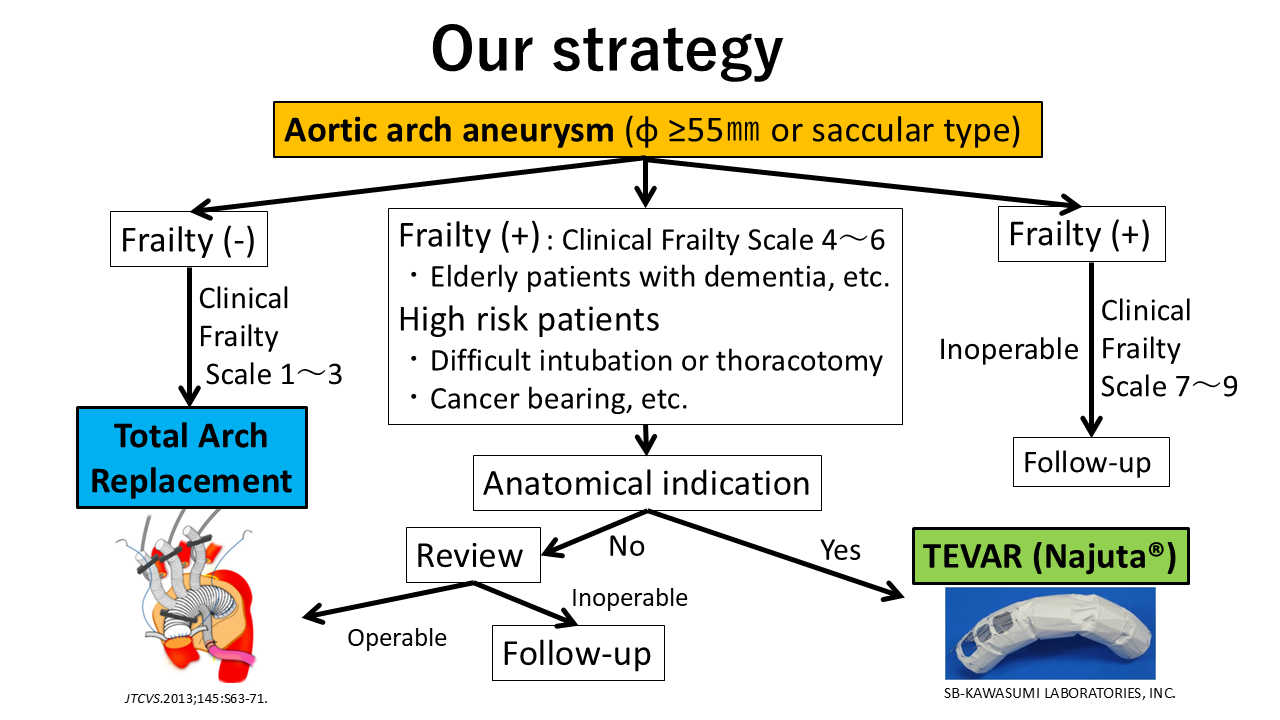
Methods: From 2011 to 2024, a total of 193 patients underwent surgery for aortic arch aneurysm: 126 patients received TAR and 67 received TEVAR with Najuta. Surgical indication was determined considering frailty and comorbidities such as cancer or respiratory dysfunction (Figure). To reduce selection bias, we used inverse probability of treatment weighting (IPTW) based on age, sex, EuroSCORE II, and frailty. Postoperative stroke and overall survival were assessed using Kaplan-Meier and Cox proportional hazards analyses.
Results: After adjustment with IPTW, the stroke rate was 2.7% (weighted N=167) in the TAR group and 16.3% (weighted N=164) in the TEVAR group, corresponding to 4 and 11 stroke cases, respectively. Logistic regression with IPTW showed that TEVAR was significantly associated with a higher risk of stroke (odds ratio 7.02, 95% CI: 2.52–19.57, p < 0.01). In Cox regression without IPTW but adjusting for age, sex, EuroSCORE II, and frailty, TEVAR was not significantly associated with reduced survival (hazard ratio 1.02, 95% CI: 0.43–2.42, p = 0.97). Male sex and frailty showed significant or borderline associations with lower survival (HR 2.74 and 2.41, p = 0.03 and 0.05, respectively). The cumulative survival rates were 84.5%, 79.0%, and 72.9% in the TAR group and 69.0%, 65.5%, and 34.0% in the TEVAR group at 3, 5, and 10 years, respectively (Log-rank p < 0.01).
Conclusions: TEVAR with Najuta, selected for high-risk patients, was associated with a significantly higher incidence of stroke even after risk adjustment. Although Kaplan-Meier curves suggested poorer survival in the TEVAR group, multivariable Cox analysis did not identify treatment type as an independent predictor of survival. These findings support the importance of individualized surgical strategy based on patient risk profiles in managing aortic arch aneurysms.
Methods: From 2011 to 2024, a total of 193 patients underwent surgery for aortic arch aneurysm: 126 patients received TAR and 67 received TEVAR with Najuta. Surgical indication was determined considering frailty and comorbidities such as cancer or respiratory dysfunction (Figure). To reduce selection bias, we used inverse probability of treatment weighting (IPTW) based on age, sex, EuroSCORE II, and frailty. Postoperative stroke and overall survival were assessed using Kaplan-Meier and Cox proportional hazards analyses.
Results: After adjustment with IPTW, the stroke rate was 2.7% (weighted N=167) in the TAR group and 16.3% (weighted N=164) in the TEVAR group, corresponding to 4 and 11 stroke cases, respectively. Logistic regression with IPTW showed that TEVAR was significantly associated with a higher risk of stroke (odds ratio 7.02, 95% CI: 2.52–19.57, p < 0.01). In Cox regression without IPTW but adjusting for age, sex, EuroSCORE II, and frailty, TEVAR was not significantly associated with reduced survival (hazard ratio 1.02, 95% CI: 0.43–2.42, p = 0.97). Male sex and frailty showed significant or borderline associations with lower survival (HR 2.74 and 2.41, p = 0.03 and 0.05, respectively). The cumulative survival rates were 84.5%, 79.0%, and 72.9% in the TAR group and 69.0%, 65.5%, and 34.0% in the TEVAR group at 3, 5, and 10 years, respectively (Log-rank p < 0.01).
Conclusions: TEVAR with Najuta, selected for high-risk patients, was associated with a significantly higher incidence of stroke even after risk adjustment. Although Kaplan-Meier curves suggested poorer survival in the TEVAR group, multivariable Cox analysis did not identify treatment type as an independent predictor of survival. These findings support the importance of individualized surgical strategy based on patient risk profiles in managing aortic arch aneurysms.
More abstracts on this topic:
Distinct Fibrochondrocyte Transdifferentiation Differentiate Thoracic Aortic Aneurysmal Remodeling from Atherogenesis
Choi Ryan, Adkar Shaunak, Leeper Nick
Active Screening in Black, Hispanic/LatinX, Asian/Pacific Islander, and Native American Individuals Reduces Racial Disparities in Abdominal Aortic Aneurysm DiagnosisMiner Grace, Govindarajulu Usha, Smolock Christopher, Faries Peter, Marin Michael