Final ID: MP901
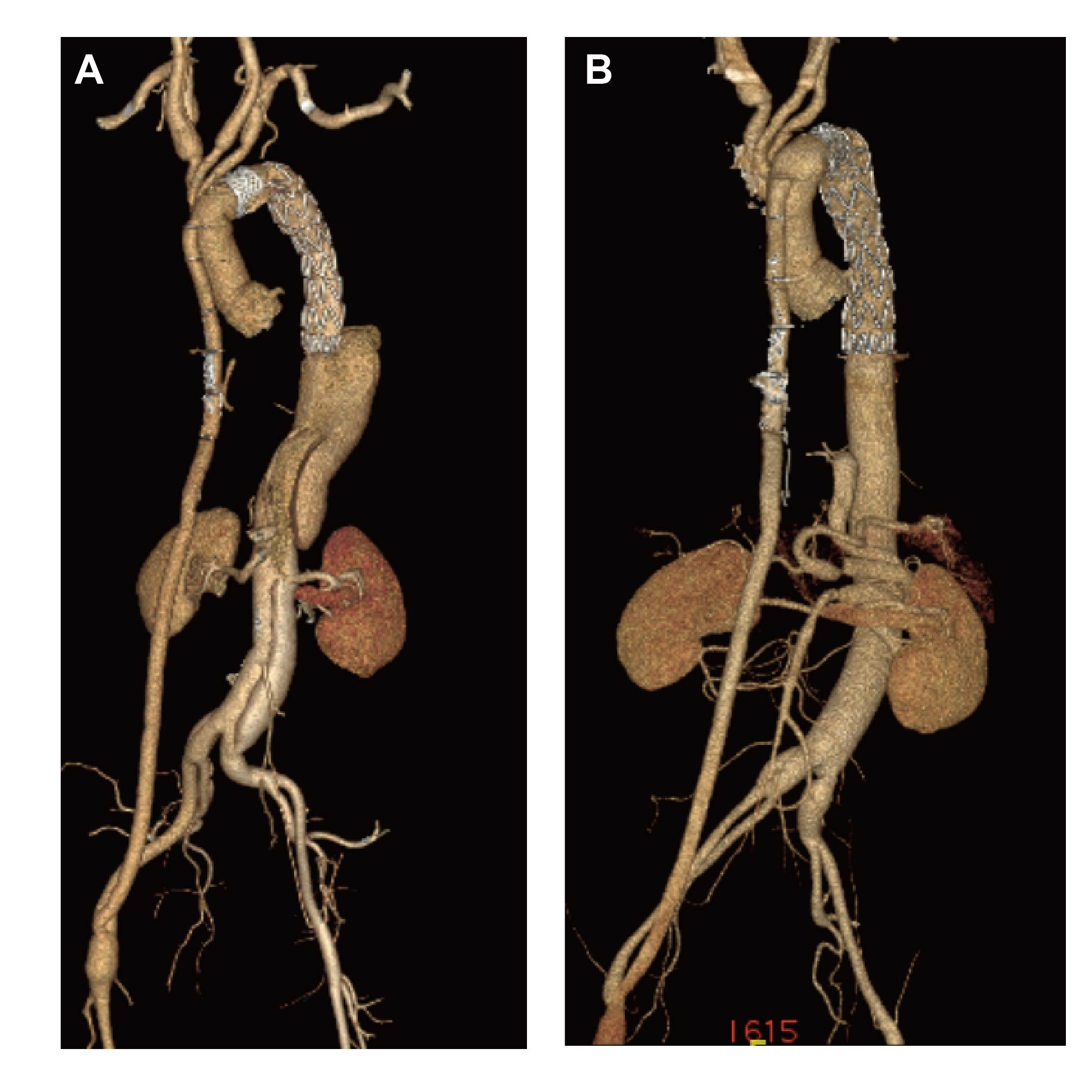
Aorta to Ilio-femoral Bypass During Total Arch Replacement with Frozen Elephant Trunk Facilitates Second-Stage Thoracoabdominal Aortic Repair with Normothermic Iliac Perfusion
Abstract Body (Do not enter title and authors here): Background: Thoracoabdominal aortic repair (TAAR) is a complex, high-risk procedure frequently performed as a second-stage operation in patients with connective tissue disorders, extensive aortic disease, or progressive disease after ascending aorta or total arch replacement (TAR) with frozen elephant trunk (FET). Aorta to ilio-femoral artery bypass (AAB) during initial TAR has been proposed to provide reliable distal perfusion and potentially optimize subsequent TAAR. However, its clinical impact remains unclear. This study aimed to evaluate the impact of AAB on early and long-term outcomes in patients undergoing staged TAAR following TAR with FET.
Methods: Patients undergoing TAAR under normothermic iliac perfusion after TAR with FET between January 2012 and December 2022 at a single center were recruited. Patients with prior thoracoabdominal surgery or thoracic endovascular aortic repair were excluded. A total of 62 patients were enrolled in the study. According to whether they received AAB in the previous TAR with FET, they were divided into group A (with AAB, n=17) and group B (without AAB, n=45). Primary endpoints were composite adverse events and long-term survival. Composite adverse events included 30-day mortality, persistent stroke, persistent paraplegia, and acute renal failure necessitating persistent continuous dialysis. Logistic regression analyses were performed to identify the predictors for adverse events.
Results: 30-day mortality (group A vs. group B: 5.9% vs. 6.7%, P = 1.000) and the incidence of composite adverse events (5.9% vs. 15.6%, P = 0.427) was low in both groups. Compared to the group B, patients in group A had significantly shorter surgery time (436.6 ± 110.8 min vs. 519.7 ± 155.1 min, P=0.048), reduced intraoperative fresh-frozen plasma transfusion [200.0 (0.0-600.0) mL vs. 600.0 (0.0-900.0) mL, P = 0.039], and shorter drainage time [10.0 (8.0-12.0) days vs. 12.0 (10.0-15.0) days, P = 0.037]. Multivariate logistic regression models confirmed that the surgery time was independent risk factors against composite adverse events (OR 1.01, 95% CI 1.00-1.02; Padj. = 0.013). Follow-up was available for 60 patients (96.8%), with a period of 52.8 ± 35.6 months. Kaplan-Meier analysis showed no significant difference in long-term survival between the two groups (log-rank P = 0.777).
Conclusions: AAB during TAR with FET ensures distal perfusion, facilitating second-stage TAAR by reducing operative time and technical difficulty.
Methods: Patients undergoing TAAR under normothermic iliac perfusion after TAR with FET between January 2012 and December 2022 at a single center were recruited. Patients with prior thoracoabdominal surgery or thoracic endovascular aortic repair were excluded. A total of 62 patients were enrolled in the study. According to whether they received AAB in the previous TAR with FET, they were divided into group A (with AAB, n=17) and group B (without AAB, n=45). Primary endpoints were composite adverse events and long-term survival. Composite adverse events included 30-day mortality, persistent stroke, persistent paraplegia, and acute renal failure necessitating persistent continuous dialysis. Logistic regression analyses were performed to identify the predictors for adverse events.
Results: 30-day mortality (group A vs. group B: 5.9% vs. 6.7%, P = 1.000) and the incidence of composite adverse events (5.9% vs. 15.6%, P = 0.427) was low in both groups. Compared to the group B, patients in group A had significantly shorter surgery time (436.6 ± 110.8 min vs. 519.7 ± 155.1 min, P=0.048), reduced intraoperative fresh-frozen plasma transfusion [200.0 (0.0-600.0) mL vs. 600.0 (0.0-900.0) mL, P = 0.039], and shorter drainage time [10.0 (8.0-12.0) days vs. 12.0 (10.0-15.0) days, P = 0.037]. Multivariate logistic regression models confirmed that the surgery time was independent risk factors against composite adverse events (OR 1.01, 95% CI 1.00-1.02; Padj. = 0.013). Follow-up was available for 60 patients (96.8%), with a period of 52.8 ± 35.6 months. Kaplan-Meier analysis showed no significant difference in long-term survival between the two groups (log-rank P = 0.777).
Conclusions: AAB during TAR with FET ensures distal perfusion, facilitating second-stage TAAR by reducing operative time and technical difficulty.
More abstracts on this topic:
C-C Chemokine Receptor Type 2 and Matrix Metalloproteinases Molecular Interaction in Rat Abdominal Aortic Aneurysm
Clickable Extracellular Vesicles for Localized Abdominal Aortic Aneurysm Repair
Zaghloul Mohamed, Elizondo Benedetto Santiago, Arif Batool, Heo Gyu Seong, Luehmann Hannah, Liu Yongjian, Gropler Robert, Sadeghi Mehran, Zayed Mohamed
Clickable Extracellular Vesicles for Localized Abdominal Aortic Aneurysm Repair
Marini Ande, Otto Ellen, Li Bo, Weinbaum Justin, Ren Xi, Campbell Phil, Curci John, Vorp David