Final ID: MP73
Purulent Pericarditis in a Patient with Haemophilus influenzae Bacteremia
Abstract Body (Do not enter title and authors here): Historically, purulent pericarditis was a recognized complication of bacterial infections, commonly due to pneumonia. However, with widespread antibiotic use it has become a rarity. It is defined as a localized infection of the pericardial space with gross or microscopic purulence and now mostly seen in cases of nosocomial bloodstream infection, thoracic surgery, and immunosuppression. Haemophilus influenzae (H influenzae), a gram-negative bacilli, is a rare cause of purulent pericarditis.
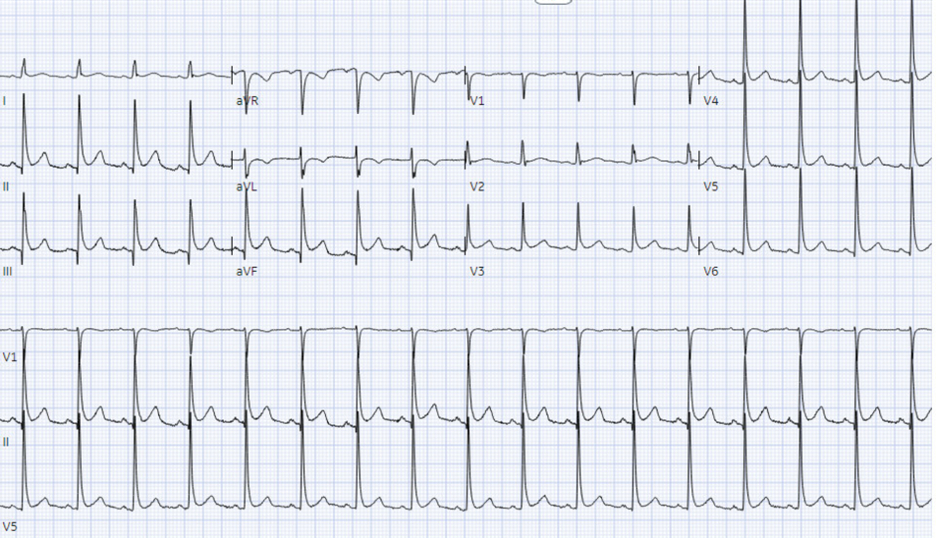
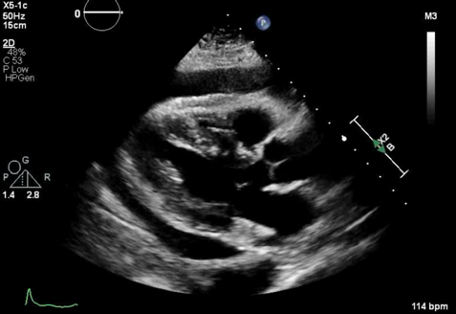
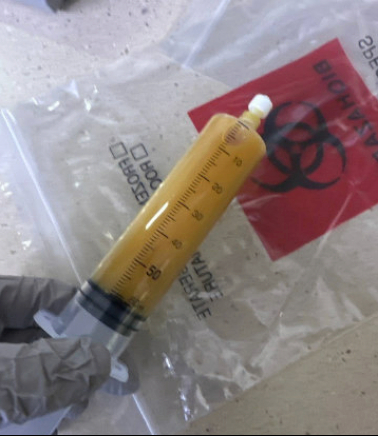
A 62-year-old female presented to the emergency room with a one-day history of non-radiating, achy chest pain worse with lying down. She was febrile at 38.4 °C and mildly tachycardic. ECG showed diffuse ST-elevation (Figure 1). Laboratory values were significant for WBC 13.6 k/μL, ESR 106 mm/hr, and CRP 30.48 mg/dL. Chest CT revealed new trace pericardial fluid or thickening possibly from trace pericardial fluid or pericarditis. Blood cultures grew H influenzae and she was started on IV ceftriaxone. She became hypotensive and echocardiogram showed normal left ventricular systolic function and a moderate-sized, circumferential pericardial effusion with compression of right ventricle consistent with tamponade (Figure 2). She underwent emergent pericardiocentesis which drained 260 mL of purulent fluid (Figure 3). Pericardial fluid studies showed WBC of 107.5 k/μL with 100% neutrophils. Pericardial fluid culture remained negative. Following initial drain removal, her hospital stay was complicated by cardiac arrest, recurrent pericardial effusions requiring repeat drain placement and a pericardial window, which resulted in a right ventricle laceration. She slowly recovered and was discharged home with a four-week course of levofloxacin.
Bacterial pericarditis caused by H influenzae is remarkably rare, regardless of strain. Purulent pericarditis is most frequently caused by Staphylococcus aureus. Presentation may include fever, dyspnea, chest pain, tachycardia, and cough. ECG may have typical findings of pericarditis with diffuse ST-segment elevation. Diagnosis is established by drainage of the pericardial fluid for culture and microscopy.
Management of purulent pericarditis is centered on adequate pericardial drainage and antimicrobials according to microbiology data. High clinical suspicion with prompt diagnosis and treatment can improve patient outcomes. Drainage options include pericardiocentesis, pericardial window, and partial or total pericardiectomy
A 62-year-old female presented to the emergency room with a one-day history of non-radiating, achy chest pain worse with lying down. She was febrile at 38.4 °C and mildly tachycardic. ECG showed diffuse ST-elevation (Figure 1). Laboratory values were significant for WBC 13.6 k/μL, ESR 106 mm/hr, and CRP 30.48 mg/dL. Chest CT revealed new trace pericardial fluid or thickening possibly from trace pericardial fluid or pericarditis. Blood cultures grew H influenzae and she was started on IV ceftriaxone. She became hypotensive and echocardiogram showed normal left ventricular systolic function and a moderate-sized, circumferential pericardial effusion with compression of right ventricle consistent with tamponade (Figure 2). She underwent emergent pericardiocentesis which drained 260 mL of purulent fluid (Figure 3). Pericardial fluid studies showed WBC of 107.5 k/μL with 100% neutrophils. Pericardial fluid culture remained negative. Following initial drain removal, her hospital stay was complicated by cardiac arrest, recurrent pericardial effusions requiring repeat drain placement and a pericardial window, which resulted in a right ventricle laceration. She slowly recovered and was discharged home with a four-week course of levofloxacin.
Bacterial pericarditis caused by H influenzae is remarkably rare, regardless of strain. Purulent pericarditis is most frequently caused by Staphylococcus aureus. Presentation may include fever, dyspnea, chest pain, tachycardia, and cough. ECG may have typical findings of pericarditis with diffuse ST-segment elevation. Diagnosis is established by drainage of the pericardial fluid for culture and microscopy.
Management of purulent pericarditis is centered on adequate pericardial drainage and antimicrobials according to microbiology data. High clinical suspicion with prompt diagnosis and treatment can improve patient outcomes. Drainage options include pericardiocentesis, pericardial window, and partial or total pericardiectomy
More abstracts on this topic:
An Unusual Case of Listeria LVAD Infection Complicated by Intracranial Catastrophe
Zviman Julieann, Mouradjian Mallory, Rovelli Richard, Leventhal Sarah, Ananthram Manjula, Ramani Gautam, Jones Niya, Griffith Bartley, Dees Lynn, Nevin Amanda, Crowell Leigha, Soares Cullen, Amoroso Anthony
An Unlikely Host: A Rare Case of Streptococcus Pneumoniae Purulent Pericarditis in an Immunocompetent PatientAbdel Aziz Khaled, Tejan Sie Ahmad, Sabbagh Abboud, Sultan Hamza, Slifer Damian, Khan Sarah, Sukhija Rishi