Final ID: HCM3
Impact of Mavacamten and Disopyramide on Left Ventricular Mechanical Dispersion and Ventricular Arrhythmia in Obstructive Hypertrophic Cardiomyopath
Abstract Body (Do not enter title and authors here): Background: Obstructive hypertrophic cardiomyopathy (oHCM) is characterized by left ventricular (LV) hypertrophy and outflow tract (LVOT) obstruction, increasing the risk of life-threatening ventricular arrhythmias (ltVA), including sustained ventricular tachycardia and sudden cardiac arrest. While both mavacamten and disopyramide reduce LVOT gradients, their impact on LV remodeling and arrhythmic risk remains unclear.
Research question/hypothesis: Do mavacamten and disopyramide, two agents with negative inotropic effects, differ in their electromechanical impact in patients with oHCM? We hypothesized that mavacamten would reduce LVMD, improve myocardial work indices, and lower the incidence of ltVA compared to disopyramide, and that lower LVMD would be associated with reduced ltVA events.
Methods: We retrospectively analyzed 120 oHCM patients treated with mavacamten (n=47) or disopyramide (n=73). LV remodeling was assessed using echocardiographic speckle-tracking before and after treatment (median 12 months (range: 6-24)). Patients were followed for 2 years for ltVA events (Holter, loop recorder, or ICD interrogations). Age and sex matching (1:1) resulted in 40 mavacamten and 40 disopyramide patients.
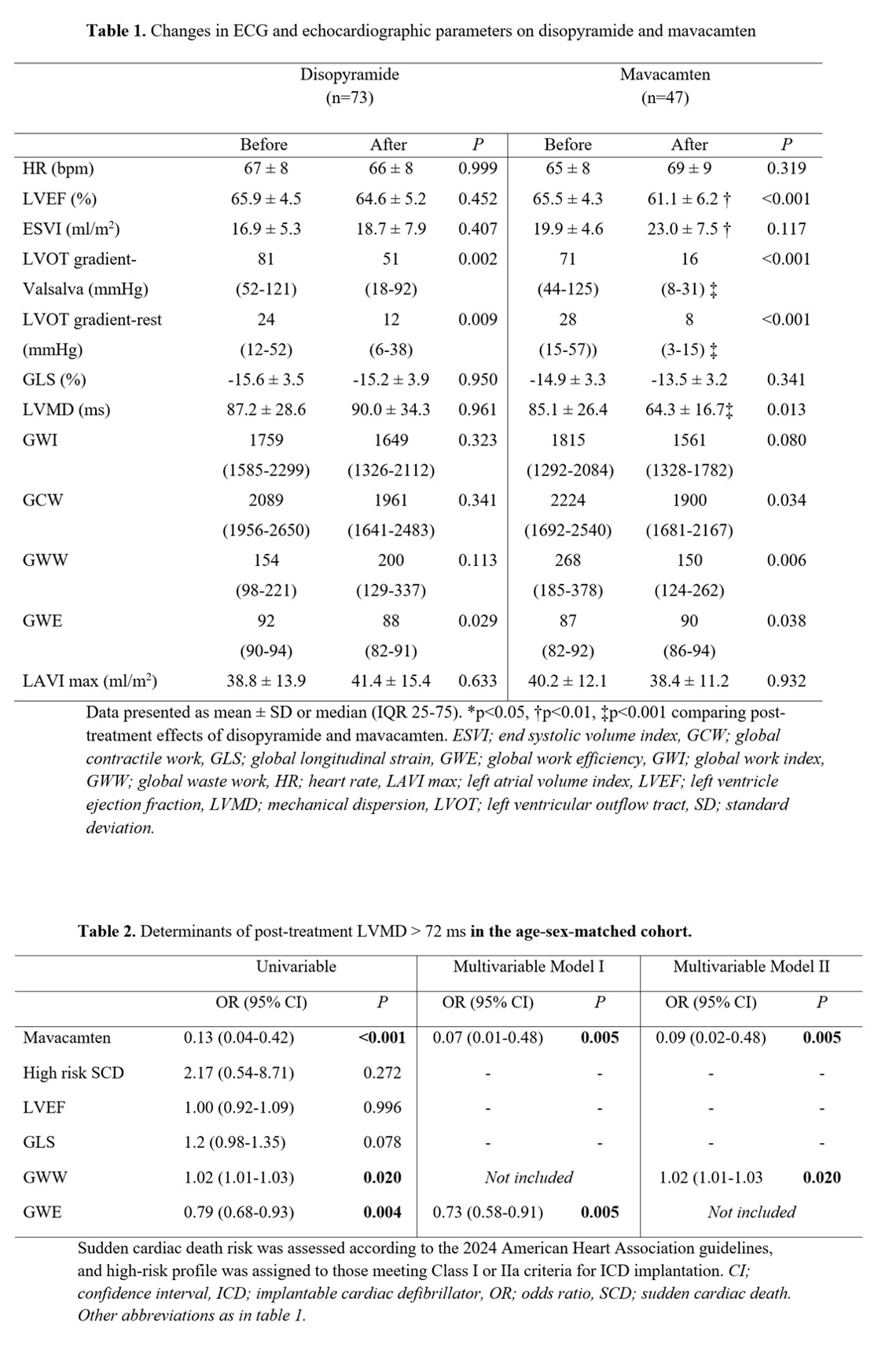
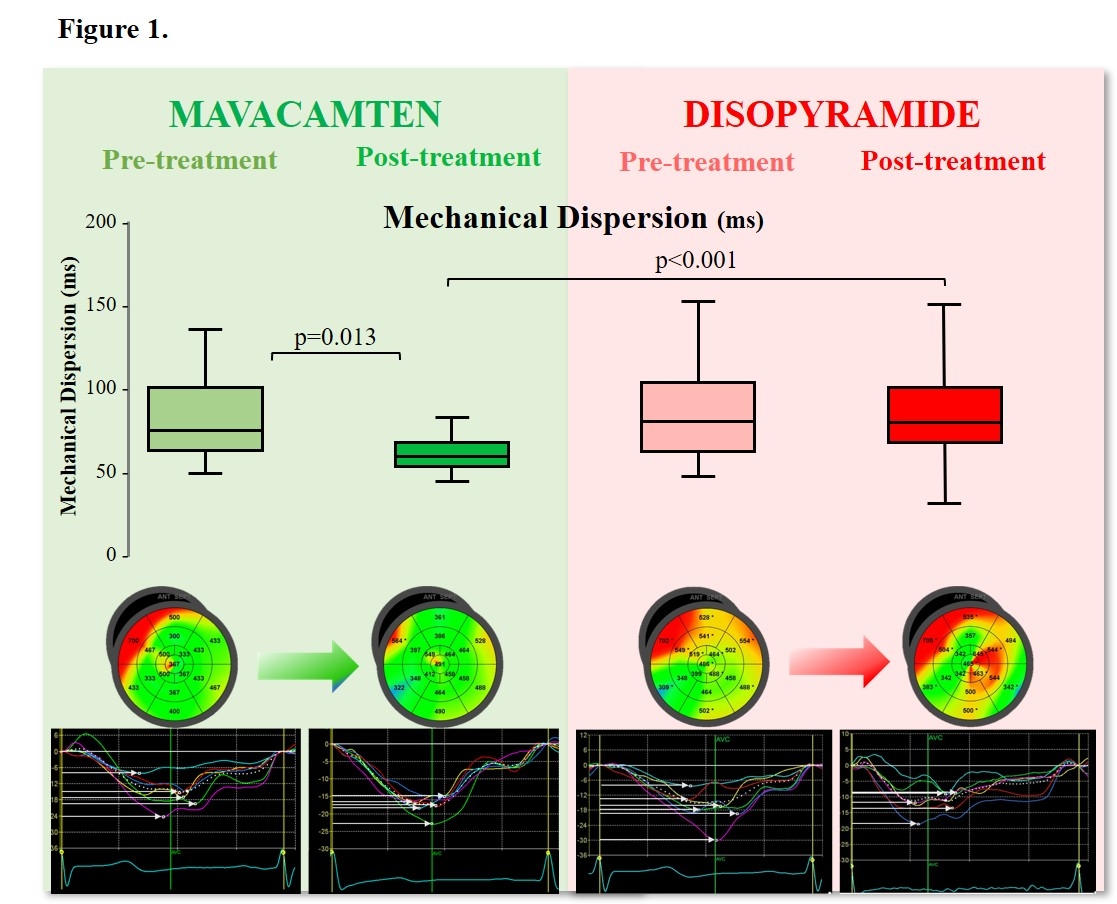
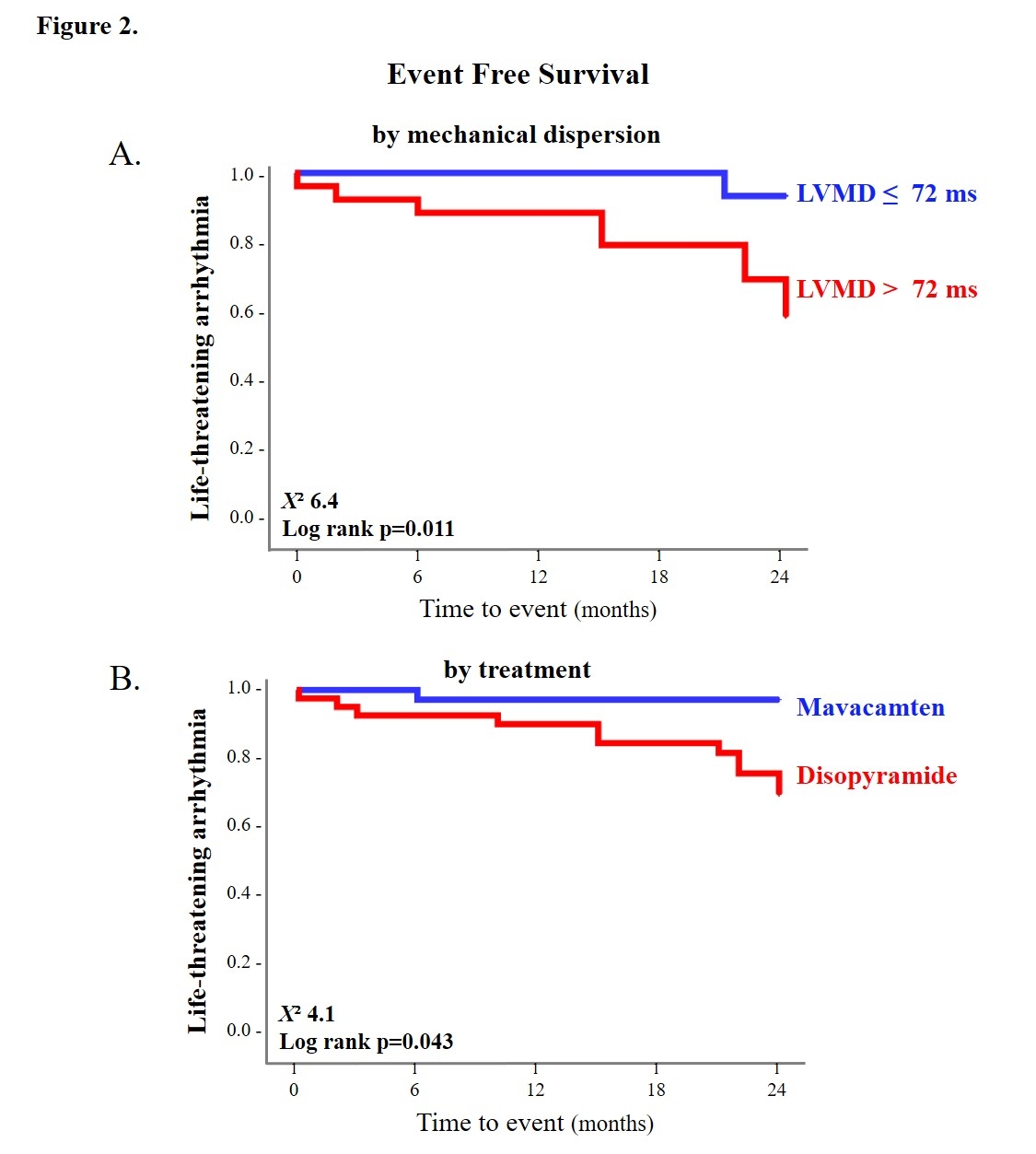
Results: Mavacamten significantly reduced LVMD (p=0.013), global wasted work (GWW) (p=0.006), and improved global work efficiency (p=0.038), while disopyramide had no significant effect on these indices (Table 1, Figure 1). In the matched cohort, over a median follow-up of 19 months, 11 ltVA events (10 ventricular tachycardia, 1 sudden cardiac arrest) occurred in the disopyramide group versus 1 ventricular tachycardia in the mavacamten group (p=0.002). Post-treatment LVMD >72 ms was linked to higher ltVA rates (p<0.001), and mavacamten was associated with LVMD independently of age, myocardial work indices, and high-risk sudden cardiac arrest profile (Table 2). LVMD ≤72 ms (p=0.011) was associated with lower ltVA risk (Figure 2).
Conclusion: Mavacamten improved LV remodeling by reducing LVMD and GWW, and was associated with fewer ltVA events in contrast to disopyramide.
Research question/hypothesis: Do mavacamten and disopyramide, two agents with negative inotropic effects, differ in their electromechanical impact in patients with oHCM? We hypothesized that mavacamten would reduce LVMD, improve myocardial work indices, and lower the incidence of ltVA compared to disopyramide, and that lower LVMD would be associated with reduced ltVA events.
Methods: We retrospectively analyzed 120 oHCM patients treated with mavacamten (n=47) or disopyramide (n=73). LV remodeling was assessed using echocardiographic speckle-tracking before and after treatment (median 12 months (range: 6-24)). Patients were followed for 2 years for ltVA events (Holter, loop recorder, or ICD interrogations). Age and sex matching (1:1) resulted in 40 mavacamten and 40 disopyramide patients.
Results: Mavacamten significantly reduced LVMD (p=0.013), global wasted work (GWW) (p=0.006), and improved global work efficiency (p=0.038), while disopyramide had no significant effect on these indices (Table 1, Figure 1). In the matched cohort, over a median follow-up of 19 months, 11 ltVA events (10 ventricular tachycardia, 1 sudden cardiac arrest) occurred in the disopyramide group versus 1 ventricular tachycardia in the mavacamten group (p=0.002). Post-treatment LVMD >72 ms was linked to higher ltVA rates (p<0.001), and mavacamten was associated with LVMD independently of age, myocardial work indices, and high-risk sudden cardiac arrest profile (Table 2). LVMD ≤72 ms (p=0.011) was associated with lower ltVA risk (Figure 2).
Conclusion: Mavacamten improved LV remodeling by reducing LVMD and GWW, and was associated with fewer ltVA events in contrast to disopyramide.
More abstracts on this topic:
Education for Post-Acute Stroke Patients
Schmidt Joelle, Schweers Amy
Acute Cardiac Function Change After Catheter Ablation of Ventricular Arrhythmias in Patients with Arrhythmogenic Right Ventricular CardiomyopathyDavis Nathaniel, Asirvatham Samuel, Friedman Paul, Killu Ammar, Ezzeddine Fatima, Sugrue Alan, Siontis Konstantinos, Kapa Suraj, Kowlgi Gurukripa, Giudicessi John, Bois John, Chang Ian C