Final ID: MP2545
Association of Race with Disease Expression and Clinical Outcomes among Patients with Mitral Valve Prolapse
Abstract Body (Do not enter title and authors here): Background: We do not clearly understand racial differences in risk profile, cardiac echocardiographic metrics among mitral valve prolapse (MVP) patients neither are differences in long-term outcome well characterized.
Objective: To assess the association between race, echocardiographic parameters, and clinical outcomes among MVP patients.
Methods: Baseline demographics, self reported race, echocardiographic data, medication use, and cardiovascular and medical comorbidities were evaluated for white and black patients with echocardiographic evidence of MVP (n=7751) at a large multi-hospital academic health system between 2010-2024. Patients with mitral and aortic valve procedures, mitral or aortic stenosis, infiltrative cardiomyopathies, HCM, EF<35%, and cancer were excluded. Long term outcomes regarding all-cause mortality, cardiovascular (CV) hospitalization for heart failure (HF), atrial fibrillation (AF), stroke and ventricular tachycardia/fibrillation/sudden cardiac arrest (VT/VF/SCA) were evaluated along with cardiac interventions. Multivariable Cox proportional hazard modeling was performed to impact of race on mortality and CV hospitalization.
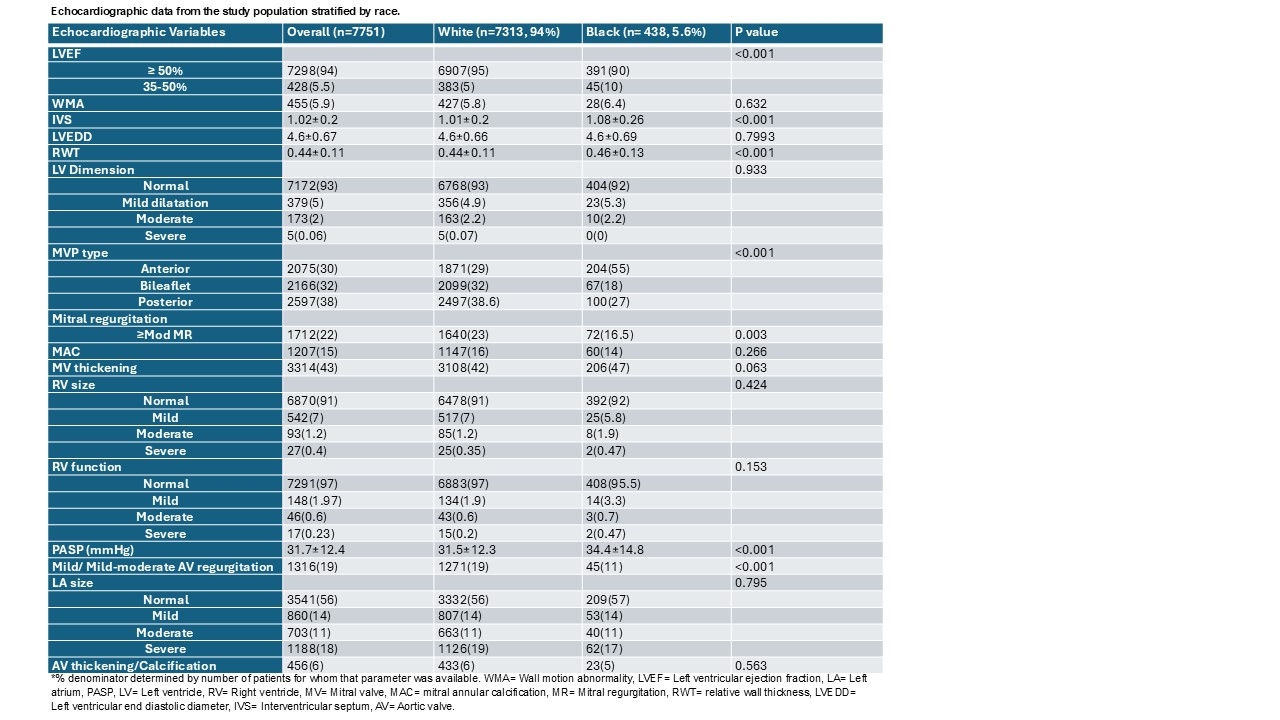
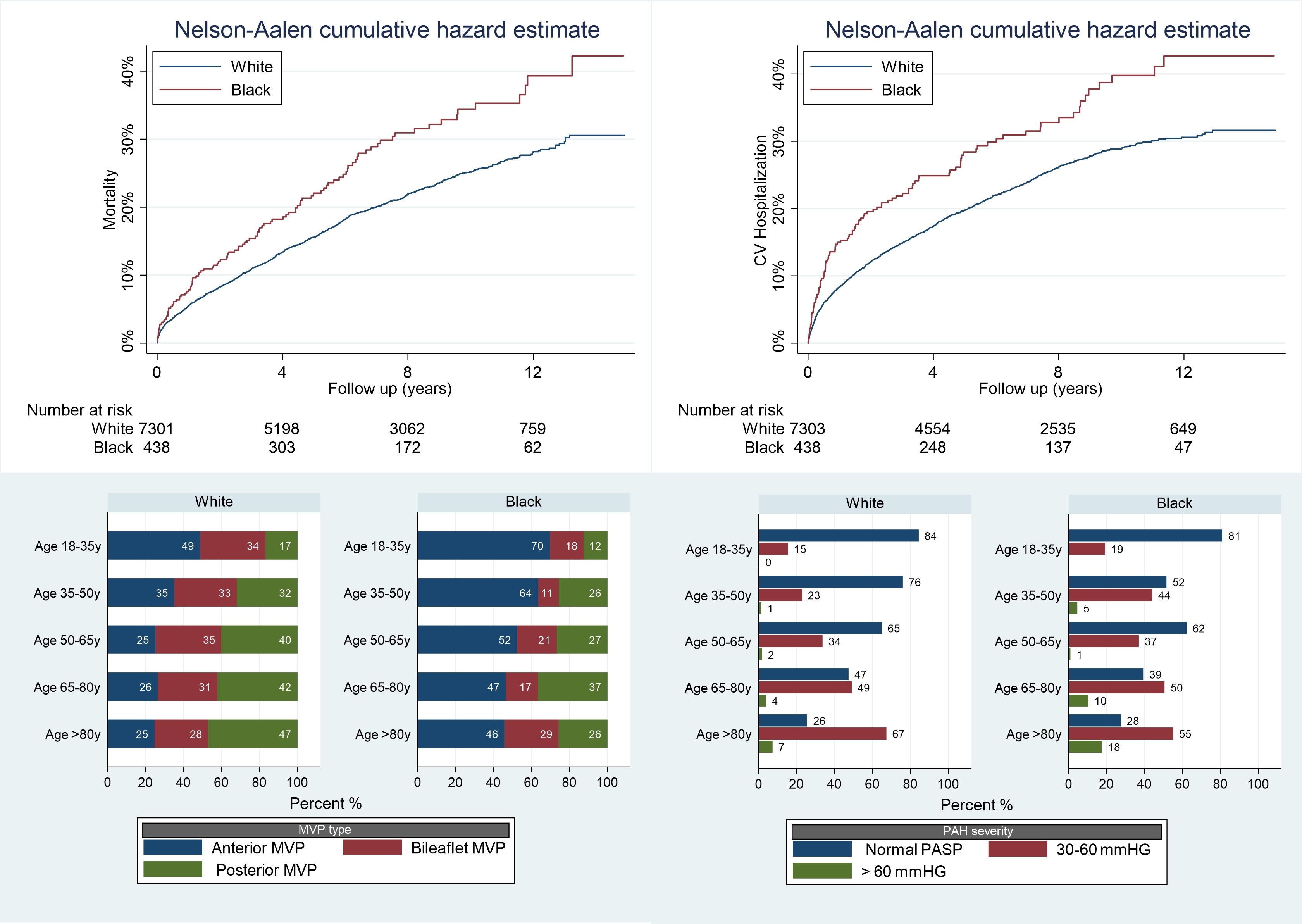
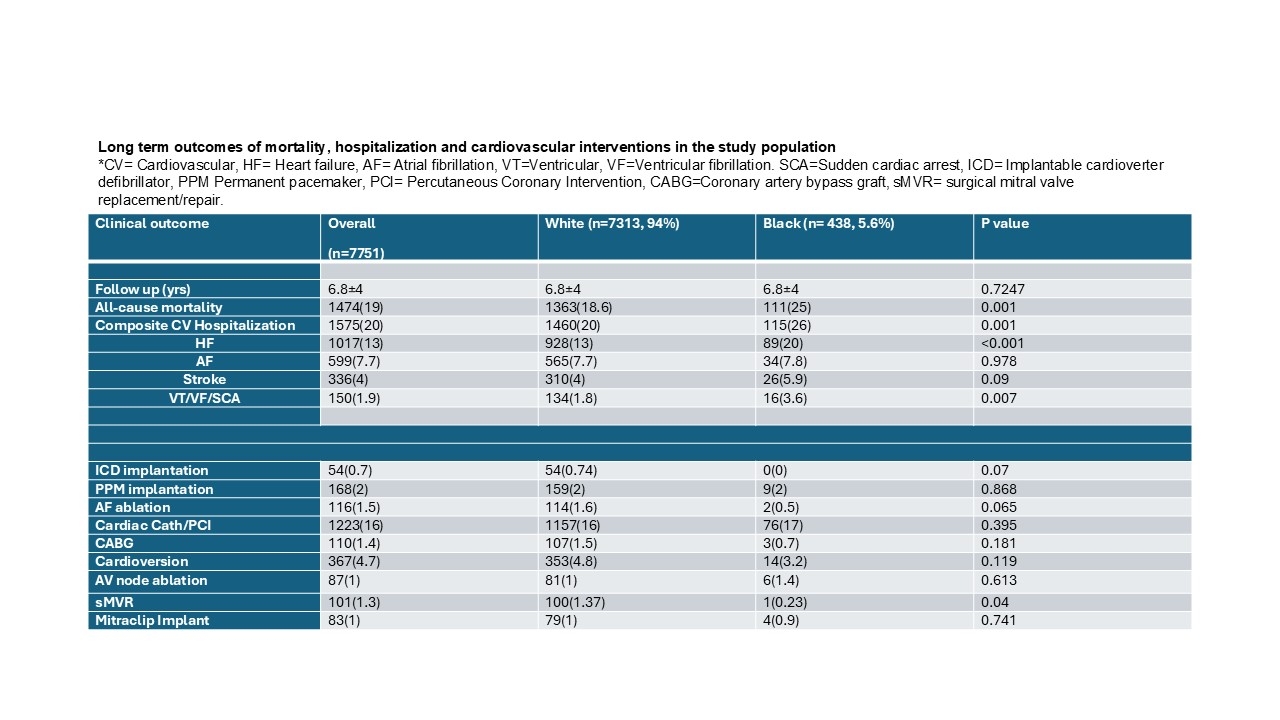
Results: Although black (n=438, 5.6%) patients with MVP were younger (57±2 vs. 62.4±2,P<0.001), they had more cardiovascular risk factors (diabetes (17% vs 7%, p<0.001), hypertension (53% vs 40%, p<0.001) chronic kidney disease (8% vs 3.4%, p<0.001)), higher comorbidity burden (Charlson Comorbidity Index 1.3±1.7 vs 0.73±1.1, p<0.001). Black patients had predominantly anterior MVP involvement (55% vs 29%) and less severe MR at presentation but had lower EF (10% with 35-50% EF) and increased pulmonary artery systolic pressures across age spectrum (Figure 1,2). Black patients experienced significantly increased comorbidity adjusted all-cause mortality (HR 1.2, CI 1-1.5, p=0.05) and CV hospitalizations (HR 1.36, CI1.1-1.6, p=0.003) particularly related to HF and VT/VF/SCA (Figure 2). However, black patients were less likely to undergo surgical mitral valve repair or ICD implantation (Figure 3).
Conclusion: Significant racial differences in disease expression, clinical outcomes and healthcare utilization exist between white and non-white mitral valve prolapse patients. Further research is needed to understand valvular phenotype and treatment gaps in MVP patients across racial and ethnic groups to improve outcomes.
Objective: To assess the association between race, echocardiographic parameters, and clinical outcomes among MVP patients.
Methods: Baseline demographics, self reported race, echocardiographic data, medication use, and cardiovascular and medical comorbidities were evaluated for white and black patients with echocardiographic evidence of MVP (n=7751) at a large multi-hospital academic health system between 2010-2024. Patients with mitral and aortic valve procedures, mitral or aortic stenosis, infiltrative cardiomyopathies, HCM, EF<35%, and cancer were excluded. Long term outcomes regarding all-cause mortality, cardiovascular (CV) hospitalization for heart failure (HF), atrial fibrillation (AF), stroke and ventricular tachycardia/fibrillation/sudden cardiac arrest (VT/VF/SCA) were evaluated along with cardiac interventions. Multivariable Cox proportional hazard modeling was performed to impact of race on mortality and CV hospitalization.
Results: Although black (n=438, 5.6%) patients with MVP were younger (57±2 vs. 62.4±2,P<0.001), they had more cardiovascular risk factors (diabetes (17% vs 7%, p<0.001), hypertension (53% vs 40%, p<0.001) chronic kidney disease (8% vs 3.4%, p<0.001)), higher comorbidity burden (Charlson Comorbidity Index 1.3±1.7 vs 0.73±1.1, p<0.001). Black patients had predominantly anterior MVP involvement (55% vs 29%) and less severe MR at presentation but had lower EF (10% with 35-50% EF) and increased pulmonary artery systolic pressures across age spectrum (Figure 1,2). Black patients experienced significantly increased comorbidity adjusted all-cause mortality (HR 1.2, CI 1-1.5, p=0.05) and CV hospitalizations (HR 1.36, CI1.1-1.6, p=0.003) particularly related to HF and VT/VF/SCA (Figure 2). However, black patients were less likely to undergo surgical mitral valve repair or ICD implantation (Figure 3).
Conclusion: Significant racial differences in disease expression, clinical outcomes and healthcare utilization exist between white and non-white mitral valve prolapse patients. Further research is needed to understand valvular phenotype and treatment gaps in MVP patients across racial and ethnic groups to improve outcomes.
More abstracts on this topic:
Cell senescence and abnormal autophagy flux contribute to mitral valve degeneration in Barlow disease
Tang Qiyu, Chester Adrian, Macrae Vicky, Corcoran Brendan
Baseline Characteristics and Outcomes of Barlow Syndrome Patients with and without Atrial FibrillationRoma Nicholas, Desai Spandan, Cohen Brett, Pattoli Megan, Miller Luke, Durkin Michael