Final ID: MP611
Hearts to Home: A Framework for Understanding and Improving Discharge Efficiency in the Pediatric Acute Care Cardiology Collaborative
Delayed discharges from pediatric acute care cardiology units causes inefficient use of hospital resources, increased healthcare costs, and family dissatisfaction. Patients often face non-medical barriers after they are deemed medically ready for discharge, and causes of delay are challenging to measure. “Medical readiness” is an evidence-based measure shown to improve discharge. “Hearts to Home” (H2H), was launched to integrate the medical readiness framework, evaluate causes of discharge delay, and improve discharge efficiency across centers in the Pediatric Acute Care Cardiology Collaborative (PAC3).
Methods:
Fourteen centers in PAC3 developed a QI initiative using the Institute for Healthcare Improvement’s Model for Improvement with the goal of decreasing the time between medical readiness and actual discharge. The SMART Aim was to increase the percentage of patients discharged within 2 hours of medical readiness to 80% by project end. Process measures included documentation of medical readiness criteria and the readiness timestamp; balancing measure was hospital readmission. Interventions included shared medical readiness definitions, rounding tools, discharge planning workflows, and barrier identification. Sites engaged in collaborative learning through monthly working group meetings, statistical process control reviews, and shared PDSA cycles.
Results:
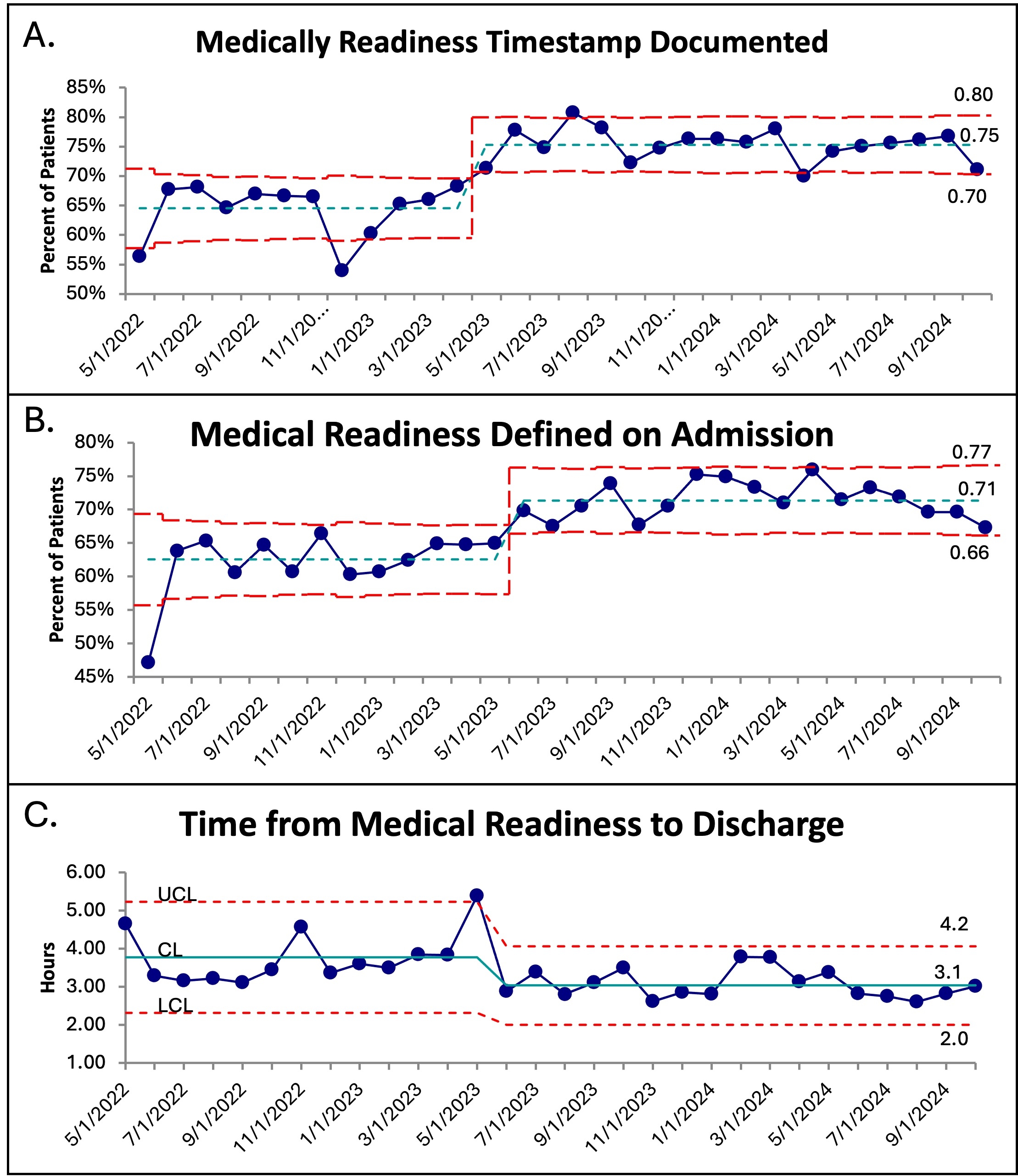
Across 22,147 discharges (May 2022—October 2024) 15,766 (71%) had a medical readiness timestamp documented. Special cause variation was achieved in documentation of medical readiness criteria on admission (Figure 1A), medical readiness timestamp (Figure 1B), and time from medical readiness to discharge with a decrease from a mean of 3.8 hours to 3.1 hours (Figure 1C). Identified causes of discharge delay included pharmacy delays (14%), transportation delays and family preference (13% each), and rounding and education delays (8% each). There was no change in 7-day readmission rates. Key drivers of success included integration of discharge discussions into daily rounds, electronic tools for capturing discharge readiness, and designated discharge roles.
Conclusions:
The H2H QI collaborative successfully implemented a framework for implementation of medical readiness to bring attention to timely discharge. Causes of discharge delays were identified and discharge efficiency was improved, though not to the SMART aim goal. Future improvement efforts will focus on specific reasons for delayed discharge.
- Ware, Adam ( UNIVERSITY OF UTAH , Salt Lake Cty , Utah , United States )
- Jensen, Megan ( Children's Mercy Hospital , Kansas City , Missouri , United States )
- Kipps, Alaina ( Stanford University , Redwood City , California , United States )
- Mclellan, Mary ( Boston Children's Hospital , Boston , Massachusetts , United States )
- Pater, Colleen ( Cincinnati Children's Hospital , Cincinnati , Ohio , United States )
- Plummer, Sarah ( Rainbow Babies and Children's Hospital , Cleveland , Ohio , United States )
- Saudek, David ( Children's Hospital Wisconsin , Madison , Wisconsin , United States )
- Schiller, Amy ( University of Michigan , Ann Arbor , Michigan , United States )
- Shah, Anar ( Stanford University , Redwood City , California , United States )
- Wehrmann, Melissa ( Nebraska Children's Hospital , Omaha , Nebraska , United States )
- Sheth, Shreya ( Baylor College of Medicine , Houston , Texas , United States )
- Birely, Alexandra ( UT Southwestern , Dallas , Texas , United States )
- Colyer, Jessica ( Seattle Childrens Hospital , Seattle , Washington , United States )
- Donaldson, Amy ( University of Pittsburgh Medical Center , Pittsburgh , Pennsylvania , United States )
- Favilla, Emmanuelle ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Figueroa, Mayte ( WUSM , St. Louis , Missouri , United States )
- Gamel, Breck ( UT Southwestern , Dallas , Texas , United States )
- Harahsheh, Ashraf ( Children's National Hospital , Washington , District of Columbia , United States )
- Higbee, Cortney ( UT Southwestern , Dallas , Texas , United States )
Meeting Info:
Session Info:
Saturday, 11/08/2025 , 10:45AM - 11:55AM
Moderated Digital Poster Session
More abstracts on this topic:
Vera-sarmiento Hernan, Qamer Syed, Jones Kelsey, Klostermann Rachel, Licari Crystal, Cresci Sharon
A novel mechanism of pediatric DCM that recapitulates aspects of the human disease via Notch signaling: a pathway to new therapeutics?Nyarko Obed, Sucharov Carmen
More abstracts from these authors:
Iguidbashian Kelsey, Plummer Sarah, Raymond Tia, Ware Adam, Patel Sonali, Buckley Jason, Church Jessica, Figueroa Mayte, Kipps Alaina, Young Jared, Kozak Nicole, Lisanti Amy, Schiller Amy
The Use of Gastrointestinal Reflux and Pro-Motility Medications in Hospitalized Infants with Congenital Heart Disease using the Pediatric Acute Care Cardiology Collaborative RegistryAlhousseiny Sara, Patel Sonali, Tiernan Kendra, Wehrmann Melissa, Harahsheh Ashraf, Frosch Olivia, Tindel Kaitlin, Plummer Sarah, Young Jared, Schiller Amy