Final ID: 4358887
Trends and Disparities in Acute Myocardial Infarction Related Mortality Among Adults with Chronic Kidney Disease in the United States, 1999–2023
Abstract Body (Do not enter title and authors here): Background: Acute myocardial infarction (AMI) in patients with chronic kidney disease (CKD) is a major health concern in U.S. adults. This study examines trends and disparities in AMI mortality among CKD patients from 1999 to 2023.
Methods: A retrospective analysis of the Centers for Disease Control and Prevention's Wide-Ranging Online Data for Epidemiological Research database examined the trends in mortality associated with AMI (ICD codes: I21, I22) in patients with CKD (ICD codes: N18). Joinpoint regression calculated age-adjusted mortality rates (AAMR) per 100,000 and annual percentage changes with 95% confidence intervals. Data were stratified by year, sex, race, age, region, and state.
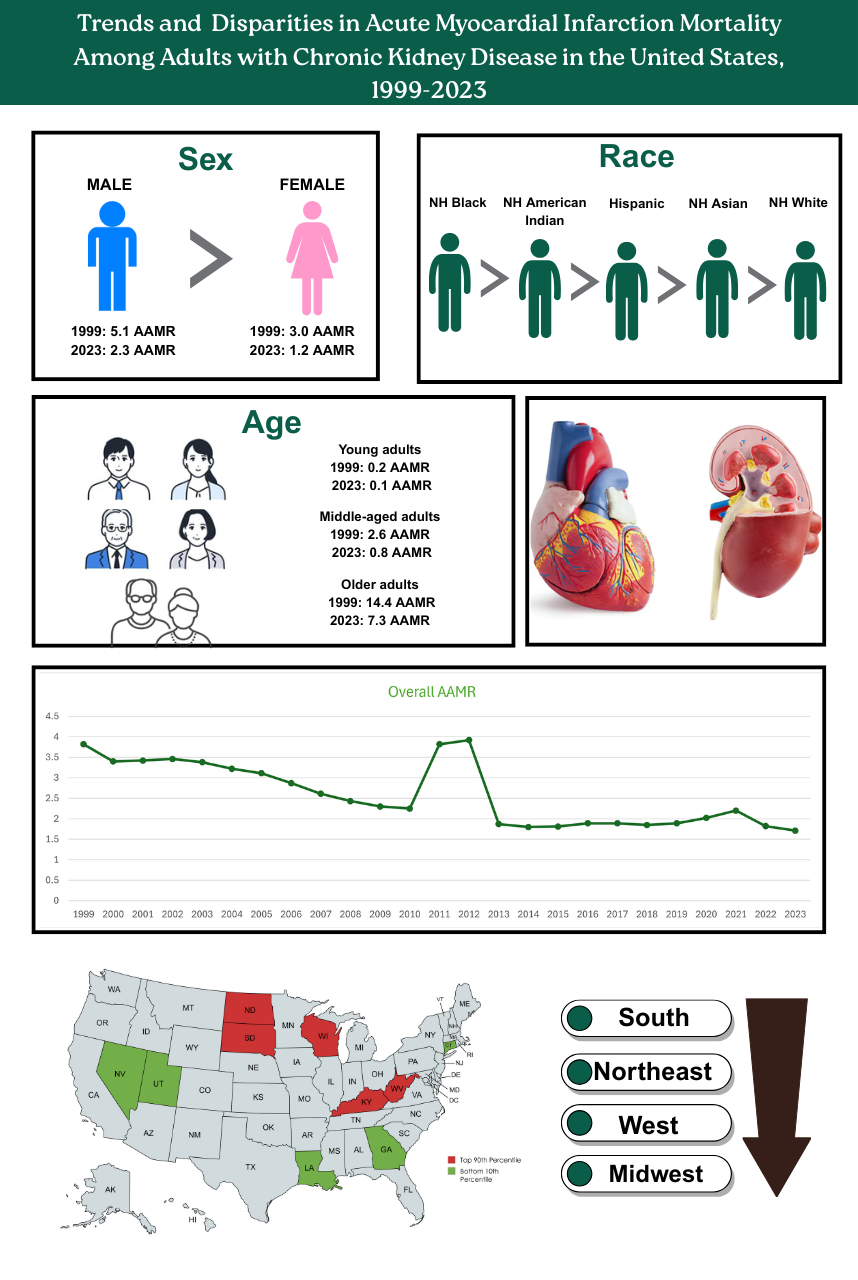
Results: Between 1999 and 2023, AMI in CKD caused 140,291 deaths. With an AAPC of -3.0% (95% CI: -4.2 to -1.9, p < 0.001), the overall AAMR decreased from 3.8 in 1999 to 1.7 in 2023. Adult men had higher AAMRs than women (men: 5.1; women: 3.0) in 1999 to (men: 2.3; women: 1.2) in 2023, with decline for both sexes [Men: AAPC: -3.0% , p < 0.001; Women: AAPC: -3.4% , p <0.001]. AAMRs varied by race, for NH Black individuals (10.4 to 2.9), NH American Indians (7.0 to 2.2), Hispanics (5.8 to 1.7), NH Asians (5.2 to 1.4), and NH Whites (2.9 to 1.5) from 1999 to 2023 respectively. AAMRs declined for all races, most notably in NH Asians (AAPC: -5.1% , p<0.001). The AAMR decreased for all age groups, for younger adults (25-44 years) it was(0.2 to 0.1) , for middle aged adults (45-64 years) (2.6 to 0.8), and for older adults(65+ years) (14.4 to 7.3) from 1999-2023 respectively, but the steepest relative decline in mortality occurred in middle aged adults (AAPC: -4.6% , p<0.001. AAMR declined in all regions—Northeast (3.7 to 1.3), Midwest (3.6 to 1.8), South (4.1 to 1.8), West (3.7 to 1.8) from 1999 to 2023 respectively, but the highest decline was seen in Northeastern region (AAPC: -3.9% , p <0.001). AAMRs varied by state, from 0.9 in Connecticut to 4.5 in North Dakota during 2023.
Conclusion: This study highlights major demographic and geographic disparities in AMI mortality among U.S. adults with CKD from 1999 to 2023. While AAMRs have declined significantly, most notably among certain racial groups and age cohorts, NH Black individuals and specific regions continue to experience disproportionately high mortality. These findings underscore the need for targeted, equity-focused strategies to reduce disparities and improve cardiovascular outcomes in AMI and CKD populations.
Methods: A retrospective analysis of the Centers for Disease Control and Prevention's Wide-Ranging Online Data for Epidemiological Research database examined the trends in mortality associated with AMI (ICD codes: I21, I22) in patients with CKD (ICD codes: N18). Joinpoint regression calculated age-adjusted mortality rates (AAMR) per 100,000 and annual percentage changes with 95% confidence intervals. Data were stratified by year, sex, race, age, region, and state.
Results: Between 1999 and 2023, AMI in CKD caused 140,291 deaths. With an AAPC of -3.0% (95% CI: -4.2 to -1.9, p < 0.001), the overall AAMR decreased from 3.8 in 1999 to 1.7 in 2023. Adult men had higher AAMRs than women (men: 5.1; women: 3.0) in 1999 to (men: 2.3; women: 1.2) in 2023, with decline for both sexes [Men: AAPC: -3.0% , p < 0.001; Women: AAPC: -3.4% , p <0.001]. AAMRs varied by race, for NH Black individuals (10.4 to 2.9), NH American Indians (7.0 to 2.2), Hispanics (5.8 to 1.7), NH Asians (5.2 to 1.4), and NH Whites (2.9 to 1.5) from 1999 to 2023 respectively. AAMRs declined for all races, most notably in NH Asians (AAPC: -5.1% , p<0.001). The AAMR decreased for all age groups, for younger adults (25-44 years) it was(0.2 to 0.1) , for middle aged adults (45-64 years) (2.6 to 0.8), and for older adults(65+ years) (14.4 to 7.3) from 1999-2023 respectively, but the steepest relative decline in mortality occurred in middle aged adults (AAPC: -4.6% , p<0.001. AAMR declined in all regions—Northeast (3.7 to 1.3), Midwest (3.6 to 1.8), South (4.1 to 1.8), West (3.7 to 1.8) from 1999 to 2023 respectively, but the highest decline was seen in Northeastern region (AAPC: -3.9% , p <0.001). AAMRs varied by state, from 0.9 in Connecticut to 4.5 in North Dakota during 2023.
Conclusion: This study highlights major demographic and geographic disparities in AMI mortality among U.S. adults with CKD from 1999 to 2023. While AAMRs have declined significantly, most notably among certain racial groups and age cohorts, NH Black individuals and specific regions continue to experience disproportionately high mortality. These findings underscore the need for targeted, equity-focused strategies to reduce disparities and improve cardiovascular outcomes in AMI and CKD populations.
More abstracts on this topic:
Atrial Fibrillation Ablation Outcomes by Hospital Academic Status: A Nationwide Comparative Analysis using TriNetX Registry
Osama Muhammad, Shabbir Muhammad Raffey, Baig Ahmad Ullah, Ahsan Waseh, Imtiaz Mahrukh
A Model-Sharing Approach for Quality Improvement of Diabetes and Cardiovascular DiseaseElligers Kyle, Pollner Meghan, Overton Katherine, Congdon Michelle, Greenway Stacey, Lambro Patricia, Sadiku Steven, Schechter Rona, Whelan John, Pressley Bianca, Sednew Renee, Duckett Sara