Final ID: MP2544
Mitral Repair Versus Mechanical Replacement in Rheumatic Patients Under 65: Outcomes in the Era of The Whole-Life Cycle for Valvular Heart Disease
Abstract Body (Do not enter title and authors here): Background:
Rheumatic mitral valve disease remains one of the most prevalent cardiovascular diseases in developing countries, affecting younger patients compared to degenerative valve disease. Evidence regarding optimal surgical strategies for rheumatic mitral valve disease patients under 65 remains limited. We aimed to quantitatively characterize valve pathology using multimodal imaging and compare midterm outcomes between two groups.
Methods:
This multicenter cohort study enrolled patients aged ≤65 years undergoing surgery between December 2016 and December 2022. All patients underwent attempted standardized SCORES repair techniques by experienced surgeons, including debridement of fibrotic commissures and leaflets, commissurotomy, subvalvular apparatus release, and annuloplasty ring implantation. Cases deemed unsuitable for repair or with suboptimal results underwent posterior leaflet-preserving mechanical valve replacement. Inverse probability weighting was used to adjust baseline differences between repair and replacement groups. Preoperative mitral valve characteristics were quantitatively assessed using multimodal imaging (echocardiography and coronary CTA).
Results:
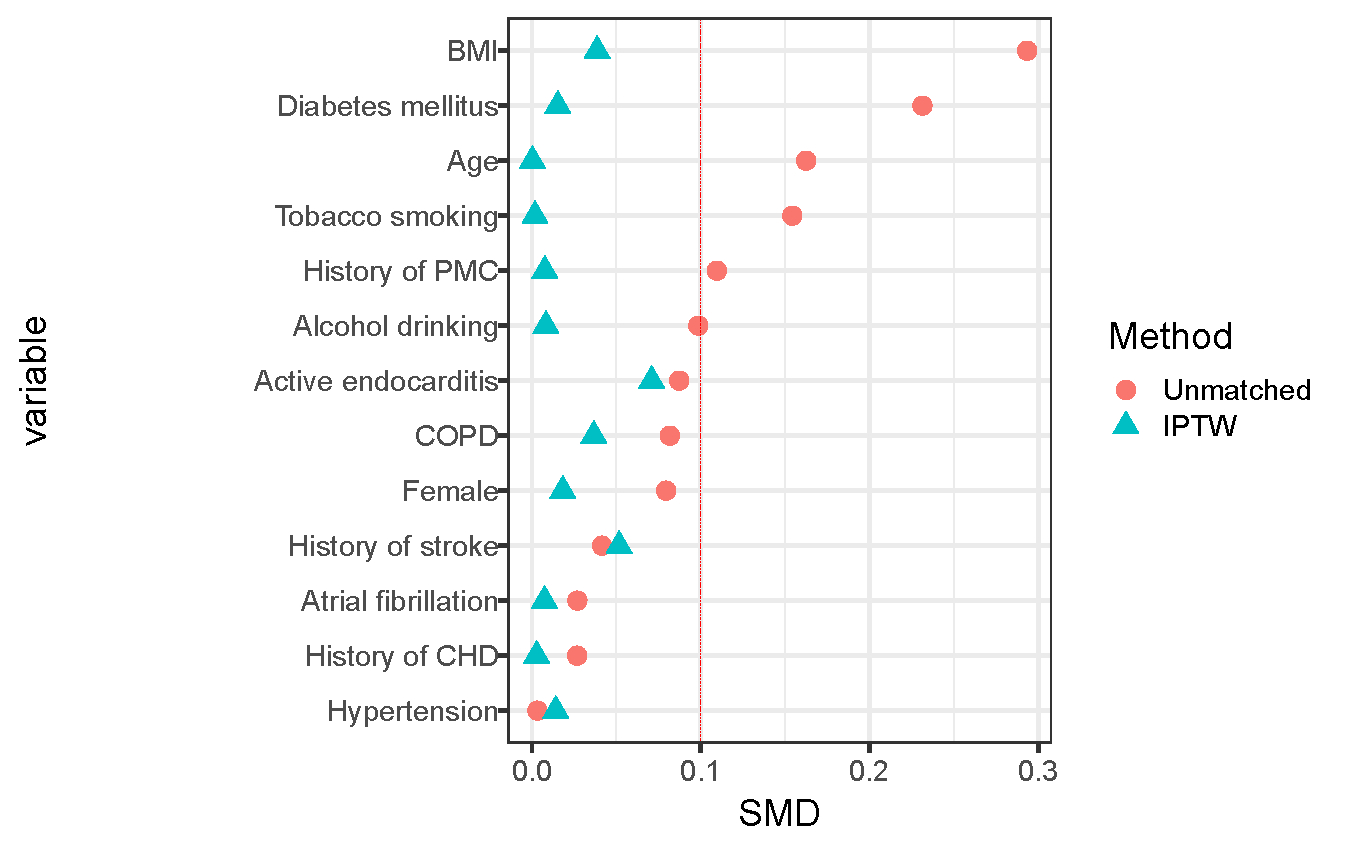
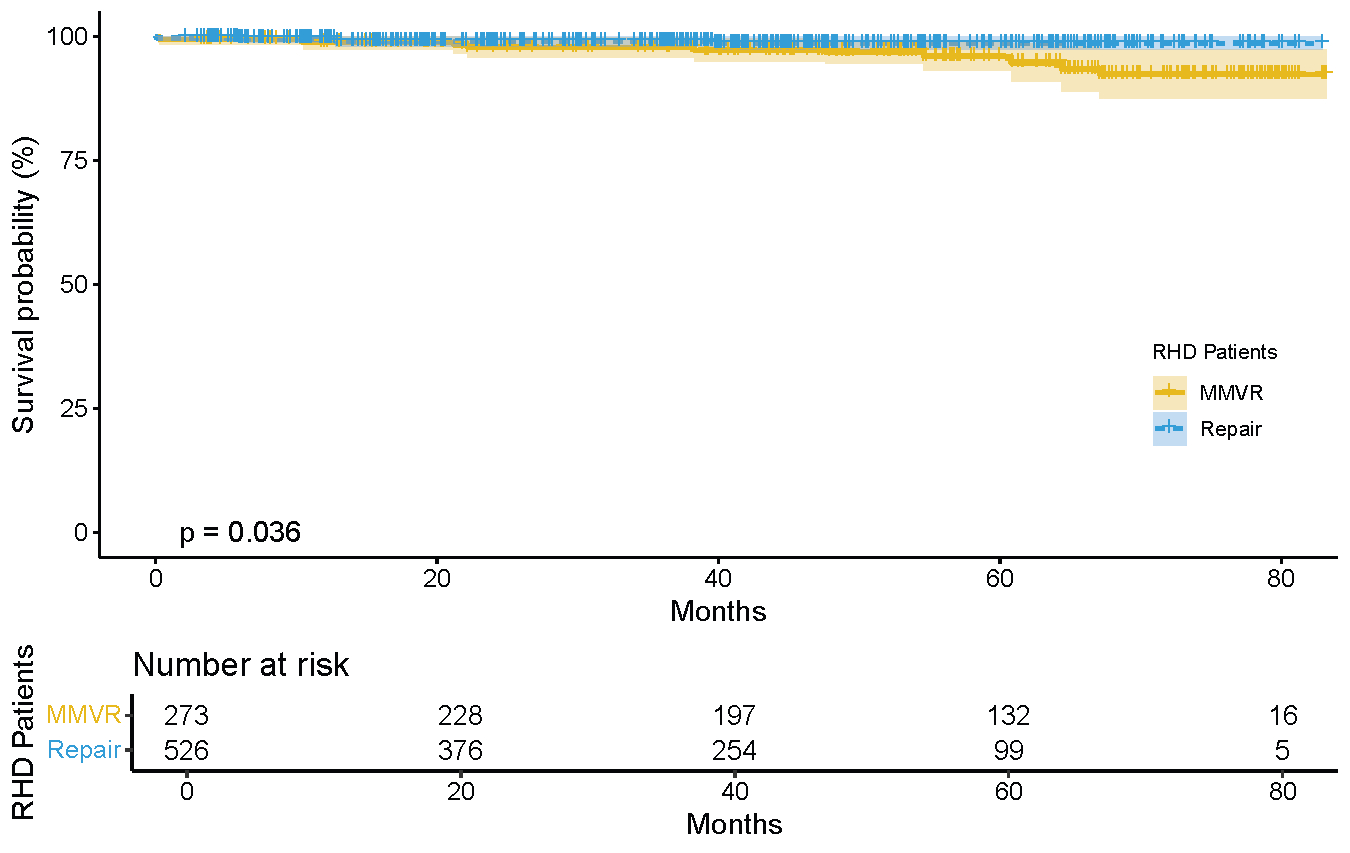
Among 799 rheumatic mitral valve disease patients under 65, 527 (66.0%) underwent repair and 272 (34.0%) underwent mechanical replacement. After inverse probability weighting (SMD<0.1 for all variables), multimodal imaging revealed lower Agatston calcium scores (0.00 vs 37.00, P<0.001), smaller left atrial diameters (50.00 vs 51.00 mm, P=0.003), and lower pulmonary artery pressures (40.00 vs 42.00 mmHg, P=0.005) in the repair group. The repair group had lower rates of postoperative respiratory failure (0.1% vs 1.3%, P=0.031) with comparable other complications. At median 43.65-month follow-up, repair demonstrated lower mortality (1.1% vs 4.9%, P=0.004), reduced stroke incidence (0.9% vs 2.8%, P=0.069), and comparable reoperation rates (0.7% vs 0.0%, P=0.167). Kaplan-Meier analysis showed significantly better midterm survival in the repair group (Log-rank P=0.036).
Conclusions:
For rheumatic mitral valve disease patients under 65, mitral valve repair significantly reduces midterm mortality and stroke risk compared to mechanical replacement, with similar reoperation rates. Future studies should evaluate long-term repair outcomes and feasibility of transcatheter reinterventions to optimize the whole-life cycle management strategies for rheumatic mitral valve disease.
Rheumatic mitral valve disease remains one of the most prevalent cardiovascular diseases in developing countries, affecting younger patients compared to degenerative valve disease. Evidence regarding optimal surgical strategies for rheumatic mitral valve disease patients under 65 remains limited. We aimed to quantitatively characterize valve pathology using multimodal imaging and compare midterm outcomes between two groups.
Methods:
This multicenter cohort study enrolled patients aged ≤65 years undergoing surgery between December 2016 and December 2022. All patients underwent attempted standardized SCORES repair techniques by experienced surgeons, including debridement of fibrotic commissures and leaflets, commissurotomy, subvalvular apparatus release, and annuloplasty ring implantation. Cases deemed unsuitable for repair or with suboptimal results underwent posterior leaflet-preserving mechanical valve replacement. Inverse probability weighting was used to adjust baseline differences between repair and replacement groups. Preoperative mitral valve characteristics were quantitatively assessed using multimodal imaging (echocardiography and coronary CTA).
Results:
Among 799 rheumatic mitral valve disease patients under 65, 527 (66.0%) underwent repair and 272 (34.0%) underwent mechanical replacement. After inverse probability weighting (SMD<0.1 for all variables), multimodal imaging revealed lower Agatston calcium scores (0.00 vs 37.00, P<0.001), smaller left atrial diameters (50.00 vs 51.00 mm, P=0.003), and lower pulmonary artery pressures (40.00 vs 42.00 mmHg, P=0.005) in the repair group. The repair group had lower rates of postoperative respiratory failure (0.1% vs 1.3%, P=0.031) with comparable other complications. At median 43.65-month follow-up, repair demonstrated lower mortality (1.1% vs 4.9%, P=0.004), reduced stroke incidence (0.9% vs 2.8%, P=0.069), and comparable reoperation rates (0.7% vs 0.0%, P=0.167). Kaplan-Meier analysis showed significantly better midterm survival in the repair group (Log-rank P=0.036).
Conclusions:
For rheumatic mitral valve disease patients under 65, mitral valve repair significantly reduces midterm mortality and stroke risk compared to mechanical replacement, with similar reoperation rates. Future studies should evaluate long-term repair outcomes and feasibility of transcatheter reinterventions to optimize the whole-life cycle management strategies for rheumatic mitral valve disease.
More abstracts on this topic:
Clinical outcomes in rheumatic mitral stenosis and the novel Yeo’s index
Leow Ryan, Li Tony, Chiu Jackie, Chan Meei-wah, Kong William, Poh Kian-keong, Kuntjoro Ivandito, Sia Ching-hui, Yeo Tiong-cheng
Cross-Platform Variations in Transthoracic Echocardiography: Implications for Clinical Decision-MakingHashemi Mohammad, Farsiani Yasaman, Pressman Gregg, Amini Mohammadreza, Kheradvar Arash