Final ID: MP2193
Prevalence of atrial fibrillation increases major adverse cardiovascular events, particularly heart failure hospitalization, in patients with peripheral arterial disease
Abstract Body (Do not enter title and authors here): Background: Peripheral arterial disease (PAD) is a leading cause of atherosclerotic disease mortality, with prevalence estimated to be 11% in the US. Studies have found that major adverse cardiovascular events (MACE) are increased in PAD patients, particularly in the presence of atherosclerotic cardiac diseases. However, whether cardiac arrhythmic diseases such as atrial fibrillation (AF) also increase this risk is unknown. We sought to determine, in a PAD population, whether the presence of AF, compared to its absence, increases the risk of MACE (all-cause death, myocardial infarction, hospitalization for heart failure [HF], stroke, and hospitalization for unstable angina).
Methods: The Intermountain Health data from Jan 2006 to Dec 2021 was used to identify adult patients with a first-time PAD diagnosis and having a second visit within 18-months (n=7613; 98.8% with symptomatic PAD). Outcomes were examined using multivariable Cox proportional hazard regressions.
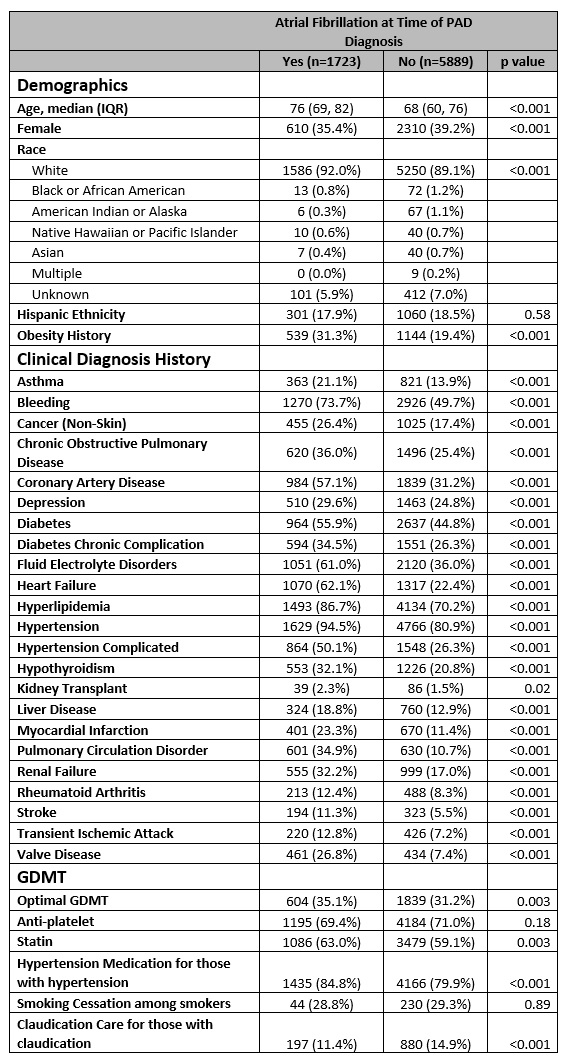
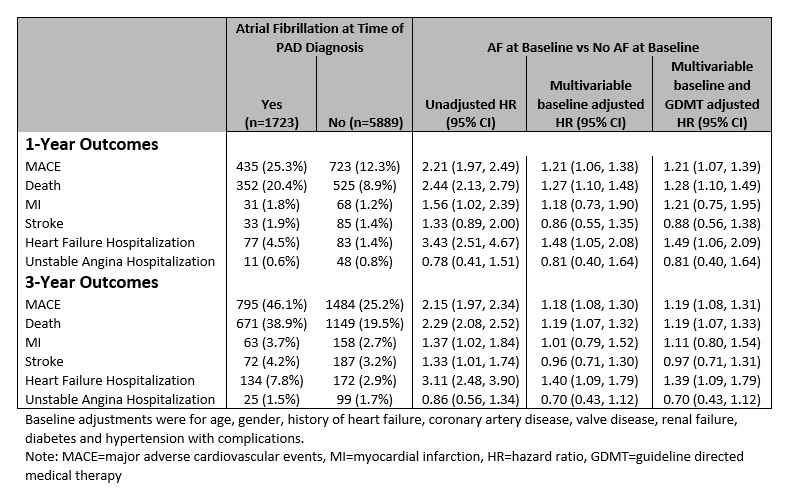
Results: A total of 1723 (22.6%) PAD patients had prior AF. The table shows differences in demographic and clinical PAD patients with and without AF. Approximately 25% of PAD patients with AF had a MACE within 1-year and 46% within 3-years compared to 12% and 25%, respectively, for those without AF. Death and HF hospitalization were the two greatest contributors to MACE. After adjustment for baseline differences and guideline-directed medical therapy (GDMT), those with AF were 21% more likely to have MACE and were 1.4-1.5 times more likely to be hospitalized for HF compared to those without AF.
Conclusions: AF was prevalent, found in a quarter of patients with PAD. The rate of MACE events was double when AF was present. After adjustment for other factors, AF patients had a 21% increased risk of MACE. HF hospitalization was a major contributor to this risk. AF should be assessed for in PAD patients and aggressive preventative treatment for MACE implemented.
Methods: The Intermountain Health data from Jan 2006 to Dec 2021 was used to identify adult patients with a first-time PAD diagnosis and having a second visit within 18-months (n=7613; 98.8% with symptomatic PAD). Outcomes were examined using multivariable Cox proportional hazard regressions.
Results: A total of 1723 (22.6%) PAD patients had prior AF. The table shows differences in demographic and clinical PAD patients with and without AF. Approximately 25% of PAD patients with AF had a MACE within 1-year and 46% within 3-years compared to 12% and 25%, respectively, for those without AF. Death and HF hospitalization were the two greatest contributors to MACE. After adjustment for baseline differences and guideline-directed medical therapy (GDMT), those with AF were 21% more likely to have MACE and were 1.4-1.5 times more likely to be hospitalized for HF compared to those without AF.
Conclusions: AF was prevalent, found in a quarter of patients with PAD. The rate of MACE events was double when AF was present. After adjustment for other factors, AF patients had a 21% increased risk of MACE. HF hospitalization was a major contributor to this risk. AF should be assessed for in PAD patients and aggressive preventative treatment for MACE implemented.
More abstracts on this topic:
A 50% or Greater Reduction in LDL-Cholesterol Is Associated with Improved Long-Term Outcomes and Lower Health Care Utilization After Myocardial Infarction - a SWEDEHEART study
Reitan Christian, Watanabe Alexandre, Bash Lori, Galvain Thibaut, Arnet Urs, Jernberg Tomas
A KLF2-BMPER-Smad1/5 checkpoint regulates high fluid shear stress-mediated artery remodelingDeng Hanqiang, Zhang Jiasheng, Schwartz Martin