Final ID: MP411
County-Level Social Disadvantage Independently Predicts Higher Risk-Adjusted Heart Failure Hospitalization Rates in the United States
Abstract Body (Do not enter title and authors here): Background:
Heart failure (HF) is a major cause of morbidity and hospitalization in the United States. Place-based social determinants of health, including community-level vulnerability and deprivation, influence cardiovascular disease prevalence, risk factors, and outcomes, but their association with heart failure hospitalizations (HFH) has not been extensively studied. We examined the relationship between county-level social disadvantage indices [Social Vulnerability Index (SVI) and the Social Deprivation Index (SDI)] and risk-adjusted HFH rates (RA-HFHR) in the US from 2020 to 2022.
Methods:
In this retrospective study, county-level RA-HFHR data for persons aged ≥18 years obtained from the Agency for Healthcare Research and Quality were linked to their corresponding 2022 SVI data (obtained from the CDC) and the 2019 SDI data (https://www.graham-center.org/maps-data-tools/social-deprivation-index.html). These indices are computed from sociodemographic factors from the American Community Survey. SVI and SDI scores were assigned percentile scores, with higher values indicating greater social disadvantage. The linked dataset was divided into four quartiles (1st quartile [Q1] and least vulnerable or deprived, and 4th quartile [Q4] and most vulnerable/deprived). RA-HFHR per 100,000 with 95% confidence intervals (CI) were computed for each quartile and then stratified by age (18-44, 45-64, ≥65 years) and gender. A negative impact by SVI or SDI was characterized by a higher RA-HFHR in Q4 than in Q1, with non-overlapping CI. Rate differences (excess or fewer hospitalizations per 100,000) were derived by obtaining the differences between Q4 and Q1.
Results:
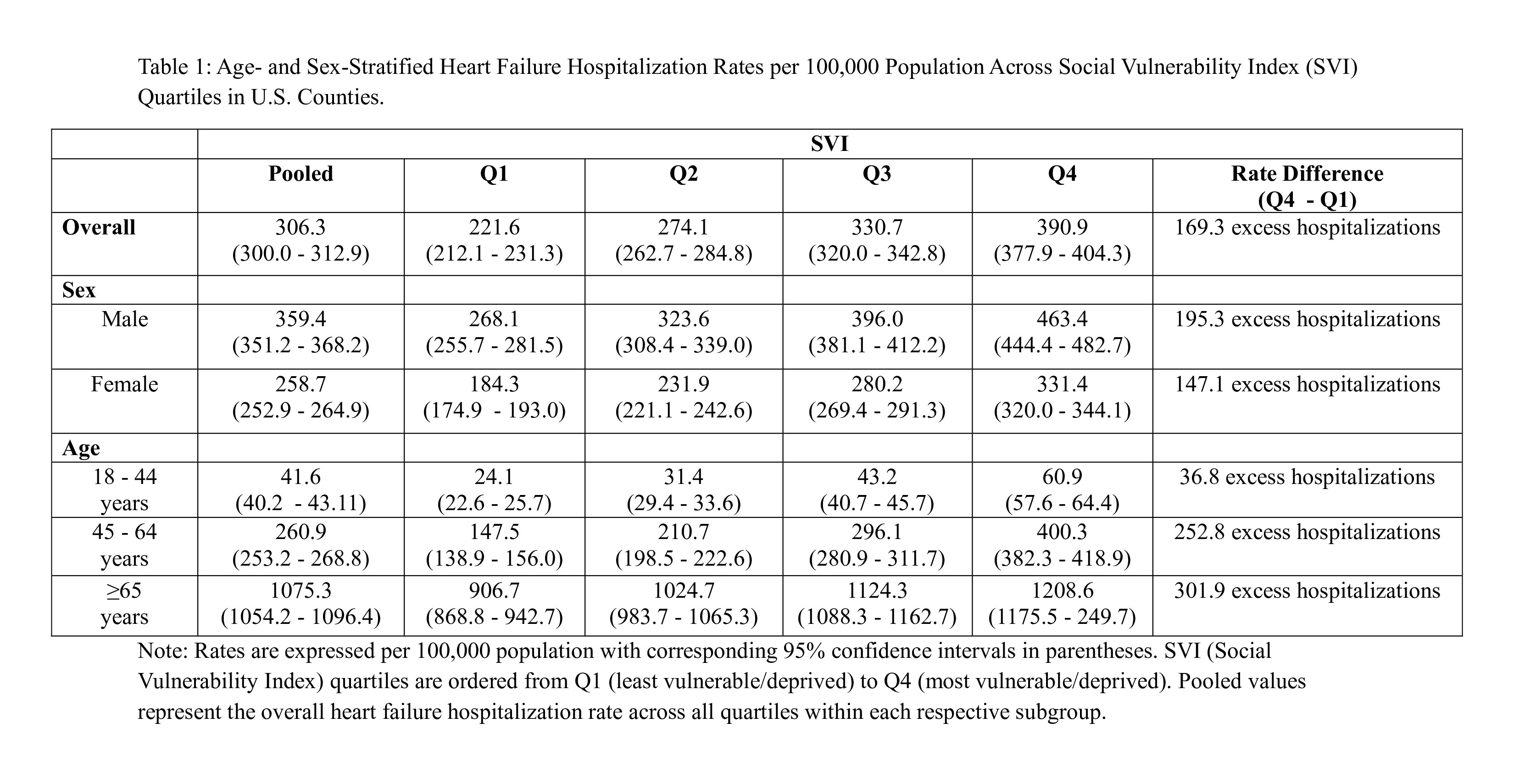
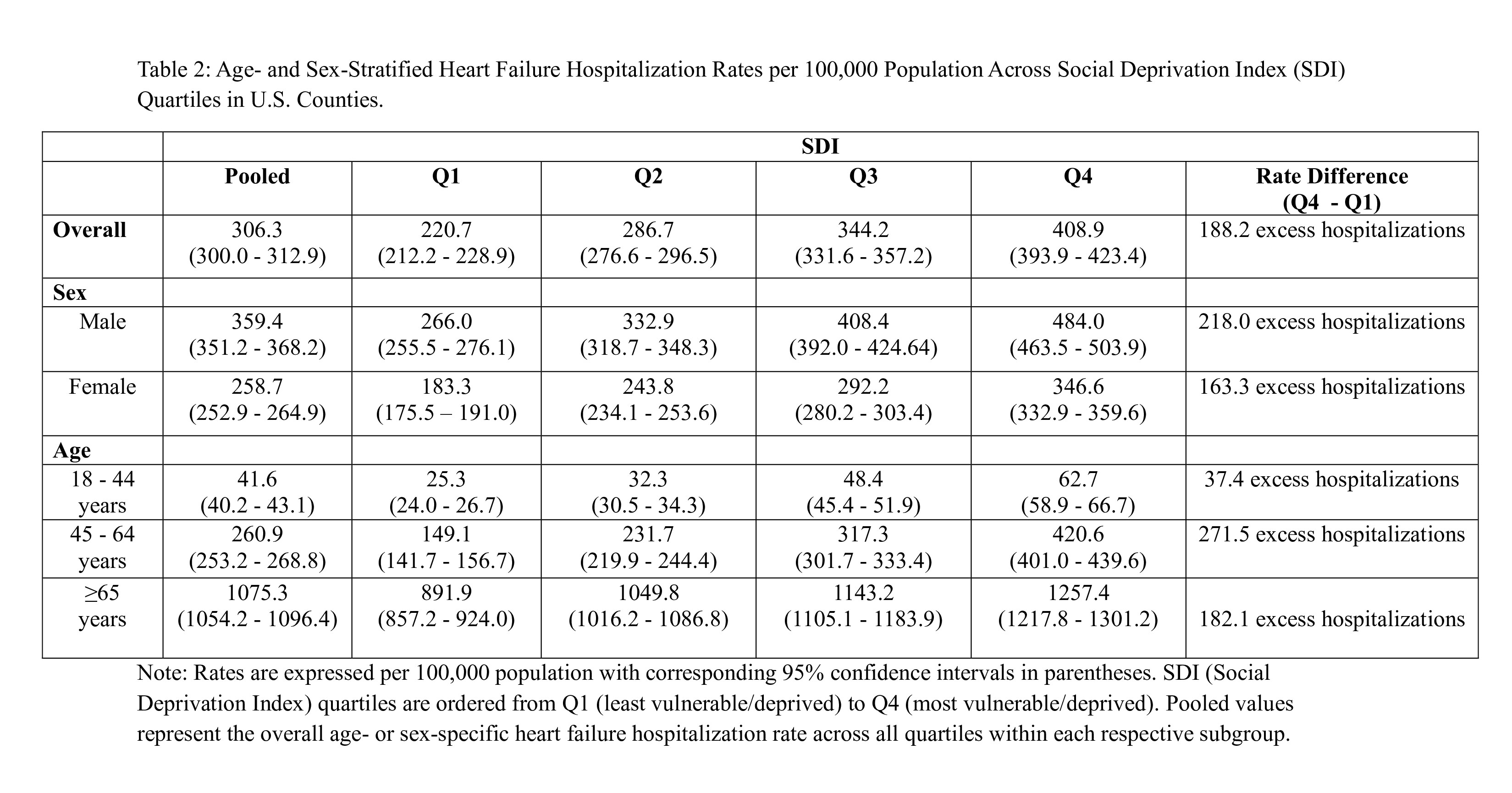
A total of 1905 counties from 33 states (>70% of the US population) were included. For SVI, the RA-HFHR increased in a stepwise manner from Q1 221.6 (CI: 212.1-231.3) in Q1 to 390.9 (CI: 77.9-404.3) in Q4, with an excess of 169.3 in Q4. The trend was similar in both genders and across all age groups (Table 1). Similarly, for SDI, the RA-HFHR significantly and progressively from 220.7 (CI: 212.2-228.9) in Q1 to 408.9 (CI: 393.9-423.4) in Q4, yielding an excess of 188.2 in Q4. Again, the trend was similar in both genders and across all age groups (Table 2).
Conclusion:
Counties with higher social vulnerability and deprivation are associated with higher RA-HFHRs. The inclusion of these indices in risk prediction models could help identify patients with HF at high risk of getting hospitalized.
Heart failure (HF) is a major cause of morbidity and hospitalization in the United States. Place-based social determinants of health, including community-level vulnerability and deprivation, influence cardiovascular disease prevalence, risk factors, and outcomes, but their association with heart failure hospitalizations (HFH) has not been extensively studied. We examined the relationship between county-level social disadvantage indices [Social Vulnerability Index (SVI) and the Social Deprivation Index (SDI)] and risk-adjusted HFH rates (RA-HFHR) in the US from 2020 to 2022.
Methods:
In this retrospective study, county-level RA-HFHR data for persons aged ≥18 years obtained from the Agency for Healthcare Research and Quality were linked to their corresponding 2022 SVI data (obtained from the CDC) and the 2019 SDI data (https://www.graham-center.org/maps-data-tools/social-deprivation-index.html). These indices are computed from sociodemographic factors from the American Community Survey. SVI and SDI scores were assigned percentile scores, with higher values indicating greater social disadvantage. The linked dataset was divided into four quartiles (1st quartile [Q1] and least vulnerable or deprived, and 4th quartile [Q4] and most vulnerable/deprived). RA-HFHR per 100,000 with 95% confidence intervals (CI) were computed for each quartile and then stratified by age (18-44, 45-64, ≥65 years) and gender. A negative impact by SVI or SDI was characterized by a higher RA-HFHR in Q4 than in Q1, with non-overlapping CI. Rate differences (excess or fewer hospitalizations per 100,000) were derived by obtaining the differences between Q4 and Q1.
Results:
A total of 1905 counties from 33 states (>70% of the US population) were included. For SVI, the RA-HFHR increased in a stepwise manner from Q1 221.6 (CI: 212.1-231.3) in Q1 to 390.9 (CI: 77.9-404.3) in Q4, with an excess of 169.3 in Q4. The trend was similar in both genders and across all age groups (Table 1). Similarly, for SDI, the RA-HFHR significantly and progressively from 220.7 (CI: 212.2-228.9) in Q1 to 408.9 (CI: 393.9-423.4) in Q4, yielding an excess of 188.2 in Q4. Again, the trend was similar in both genders and across all age groups (Table 2).
Conclusion:
Counties with higher social vulnerability and deprivation are associated with higher RA-HFHRs. The inclusion of these indices in risk prediction models could help identify patients with HF at high risk of getting hospitalized.
More abstracts on this topic:
Artificial Intelligence-enhanced Electrocardiography Sex-Discordance is Associated with Cardiovascular Events and Risk Factors in Women: from the ELSA-Brasil study
Camelo Lidyane, Zeidaabadi Boroumand, Pinto Filho Marcelo, Ribeiro Antonio Luiz, Ng Fu, Brant Luisa, Sau Arunashis, Barreto Sandhi, Giatti Luana, Oliveira Clara, Paixao Gabriela, Barker Joseph, Pastika Libor, Patlatzoglou Konstantinos
Age-, Sex- and/or Ethnic- specific disparities; Biventricular systolic and diastolic strain, and biomarker, prognostic implications in Acute Tuberculous Pericarditis.Matshela Mamotabo