Final ID: MP1538
Social Vulnerability and Deprivation Indices Predict Excess Hypertension-Related Hospitalizations Across U.S. Counties
Abstract Body (Do not enter title and authors here): Background:
Prevention quality indicators in inpatient settings, such as hypertension-related hospitalizations (HRH), are population-based admissions that can be prevented through timely and effective outpatient care. However, the impact of county-level social disadvantage on HRH has not been extensively studied.
Objectives:
To examine the association between county-level social disadvantage indices [social vulnerability index (SVI) and social deprivation index (SDI)] and HRH in all US counties from 2020-2022. We hypothesized that counties with higher SVI and SDI would have higher HRH.
Methods:
In this retrospective study, county-level risk-adjusted HRH rate (RA-HRHR) data for individuals aged 18 years and older were obtained from the Agency for Healthcare Research and Quality and linked to their corresponding 2022 SVI data from the CDC. The SVI measures social drivers of health in US counties based on 16 social attributes related to socioeconomic factors, household characteristics, minority status, and housing. transportation. SVI values were assigned percentile scores, with higher values indicating greater social disadvantage. The linked dataset was divided into 4 quartiles (1st quartile [Q1] and least vulnerable, and 4th quartile [Q4] and most vulnerable). The mean RA-HRHR per 100,000 population, along with 95% confidence intervals (CI), was calculated for each quartile and subsequently stratified by age groups (18-44, 45-64, ≥65 years) and gender. A negative impact of SVI was characterized by a higher RA-HRHR in Q4 than in Q1, with non-overlapping CIs. The analysis was repeated with SDI, which is computed from 7 sociodemographic variables.
Results:
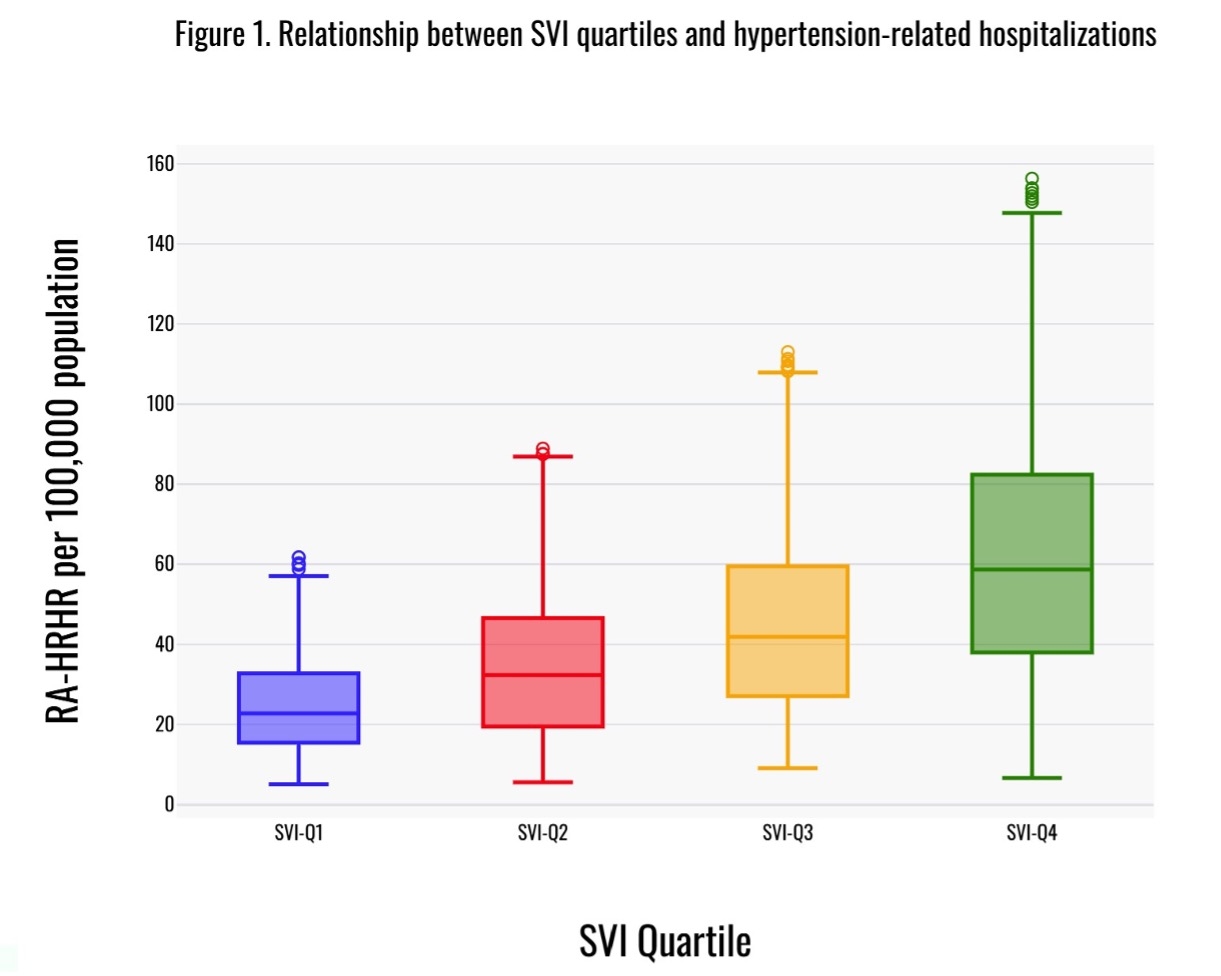
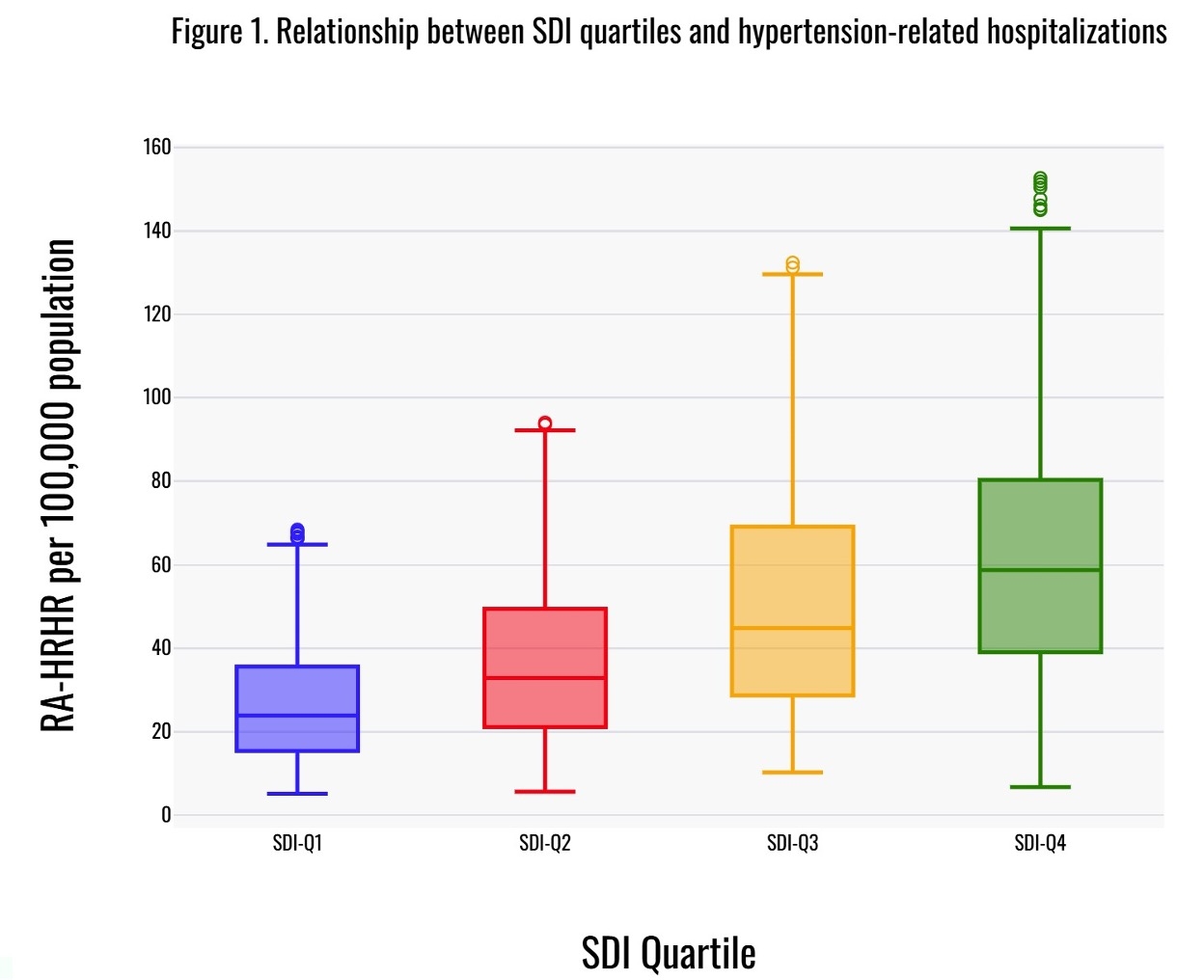
A total of 1793 counties from 33 states (>70% of the US population) were included. For SVI, the RA-HRHR increased in a stepwise manner from 27.7 (CI: 25.9-29.6) in Q1 to 67.6 (CI: 63.3-73.2) in Q4, with an excess of 39.9 in Q4 (Figure 1). The trend was similar in both genders and all age groups. Similarly, for SDI, the RA-HRHR also increased in a stepwise manner from 29.3 (CI: 27.5-31.1) in Q1 to 69.6 (CI: 64.6-76.1) in Q4, with an excess of 40.3 in Q4 (Figure 2).
Conclusion:
Higher county-level SVI and SDI are linked to increased HRH in the US, indicating that these counties may have unmet outpatient care needs. Both indices could be used as proxies for identifying persons with hypertension at high risk for HRHs.
Prevention quality indicators in inpatient settings, such as hypertension-related hospitalizations (HRH), are population-based admissions that can be prevented through timely and effective outpatient care. However, the impact of county-level social disadvantage on HRH has not been extensively studied.
Objectives:
To examine the association between county-level social disadvantage indices [social vulnerability index (SVI) and social deprivation index (SDI)] and HRH in all US counties from 2020-2022. We hypothesized that counties with higher SVI and SDI would have higher HRH.
Methods:
In this retrospective study, county-level risk-adjusted HRH rate (RA-HRHR) data for individuals aged 18 years and older were obtained from the Agency for Healthcare Research and Quality and linked to their corresponding 2022 SVI data from the CDC. The SVI measures social drivers of health in US counties based on 16 social attributes related to socioeconomic factors, household characteristics, minority status, and housing. transportation. SVI values were assigned percentile scores, with higher values indicating greater social disadvantage. The linked dataset was divided into 4 quartiles (1st quartile [Q1] and least vulnerable, and 4th quartile [Q4] and most vulnerable). The mean RA-HRHR per 100,000 population, along with 95% confidence intervals (CI), was calculated for each quartile and subsequently stratified by age groups (18-44, 45-64, ≥65 years) and gender. A negative impact of SVI was characterized by a higher RA-HRHR in Q4 than in Q1, with non-overlapping CIs. The analysis was repeated with SDI, which is computed from 7 sociodemographic variables.
Results:
A total of 1793 counties from 33 states (>70% of the US population) were included. For SVI, the RA-HRHR increased in a stepwise manner from 27.7 (CI: 25.9-29.6) in Q1 to 67.6 (CI: 63.3-73.2) in Q4, with an excess of 39.9 in Q4 (Figure 1). The trend was similar in both genders and all age groups. Similarly, for SDI, the RA-HRHR also increased in a stepwise manner from 29.3 (CI: 27.5-31.1) in Q1 to 69.6 (CI: 64.6-76.1) in Q4, with an excess of 40.3 in Q4 (Figure 2).
Conclusion:
Higher county-level SVI and SDI are linked to increased HRH in the US, indicating that these counties may have unmet outpatient care needs. Both indices could be used as proxies for identifying persons with hypertension at high risk for HRHs.
More abstracts on this topic:
Disaggregating Cardiovascular-Kidney-Metabolic Mortality among Asian Subgroups in the United States
Saleem Hira, Shahid Izza, Dong Weichuan, Nasir Khurram, Al-kindi Sadeer
A Key Role of Proximal Tubule Renin-Angiotensin System in The Kidney in The Development of Kidney Ischemia and Reperfusion InjuryLi Xiao, Hassan Rumana, Katsurada Akemi, Sato Ryosuke, Zhuo Jia