Final ID: Sa3132
Tricuspid Endocarditis with Bilateral Septic Pulmonary Emboli, Necrotizing Lung Abscesses, and Refractory Hemoptysis: A Multisystem Crisis Requiring Surgical and Endovascular Intervention
Abstract Body (Do not enter title and authors here): Background:
Tricuspid valve endocarditis is highly associated with intravenous (IV) drug use. Large, mobile vegetations increase the risk of embolization leading to complications such as pulmonary infarcts.
Case:
A 38-year-old woman with drug use disorder presented with right-sided chest pain and hemoptysis. On arrival, she was febrile (T 102.9°F), tachypneic (RR 32 rpm), hypoxic (SpO2 90% on room air), tachycardic (HR 123 bpm), and hypotensive (BP 84/50 mmHg), with multiple track marks and a systolic murmur.
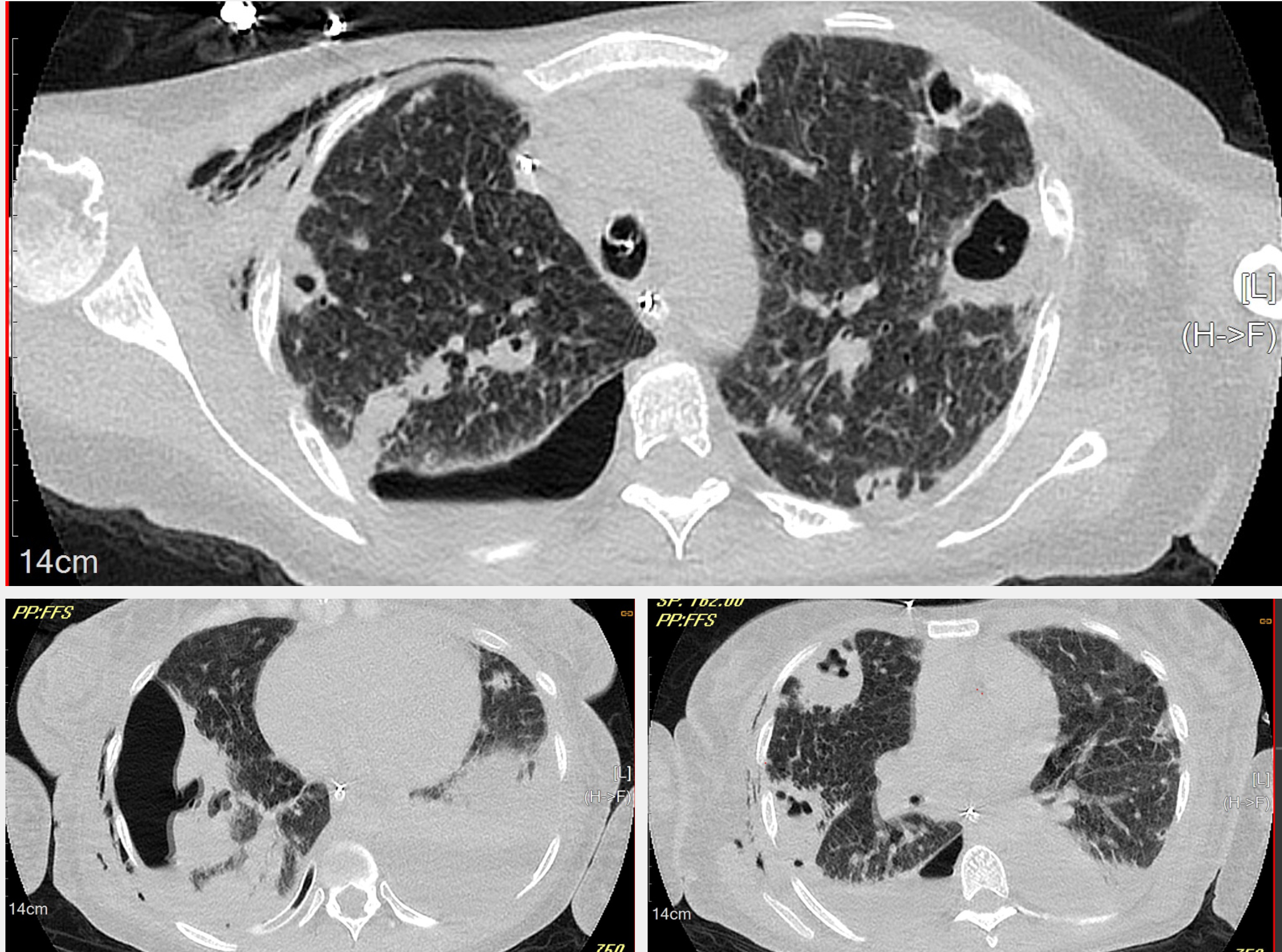
Immediate supplemental oxygen, IV fluids, pressors, and empiric antibiotics (piperacillin-tazobactam and vancomycin) were given. Laboratory studies showed elevated white cell count (WBC 18,700/μL), procalcitonin (287 ng/mL), CRP (29 mg/dL), and ESR (113 mm/h). Chest CT described bilateral pulmonary infarcts with extensive necrosis.
A 25 mm and a 24 mm vegetations on the tricuspid valve with severe regurgitation were identified on transthoracic and transesophageal echocardiography. Bacteremia by Staphylococcus aureus sensitive to vancomycin was demonstrated.
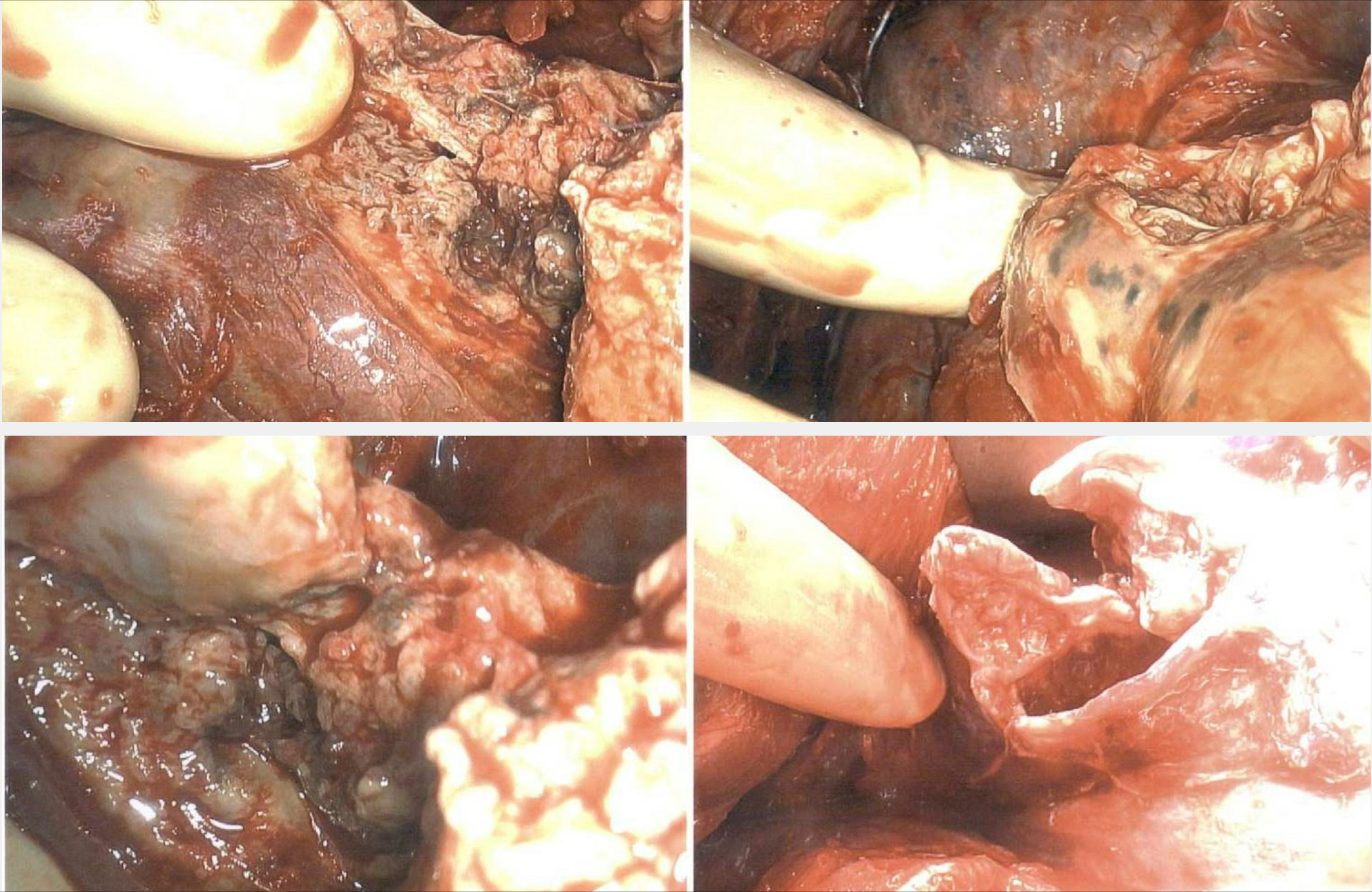
Due to a decline in the patient's respiratory status, repeat imaging was necessary, which showed a right lung abscess and empyema. She underwent video-assisted thoracoscopic surgery (VATS) with drainage and decortication.
Significant hemoptysis prompted bronchoscopy and norepinephrine injection. Persistent blood loss with hemodynamic instability was experienced, progressing into hypovolemic shock and cardiac arrest. Resuscitation was successfully performed, followed by selective arterial embolization.
High perioperative risk prevented urgent valve replacement despite having clear indications such as severe valvular dysfunction, heart failure, large mobile vegetations, and embolization. The Angiovac system using right internal jugular access, represented a suitable option for vegetation debulking allowing 80% of the mass removal. Moderate tricuspid regurgitation persisted due to residual material on the tricuspid valve leaflet.
Conclusion:
This case is an illustration of the implications of IV drug use disorders. Infective endocarditis, septic pulmonary emboli, necrotizing abscesses, and life-threatening hemoptysis are just some of the complications that patients can experience. Multidisciplinary care is critical to achieve survival in such cases. The AngioVac system is an emerging and promising technique, offering minimally invasive options for vegetation debulking in patients with high perioperative risk.
Tricuspid valve endocarditis is highly associated with intravenous (IV) drug use. Large, mobile vegetations increase the risk of embolization leading to complications such as pulmonary infarcts.
Case:
A 38-year-old woman with drug use disorder presented with right-sided chest pain and hemoptysis. On arrival, she was febrile (T 102.9°F), tachypneic (RR 32 rpm), hypoxic (SpO2 90% on room air), tachycardic (HR 123 bpm), and hypotensive (BP 84/50 mmHg), with multiple track marks and a systolic murmur.
Immediate supplemental oxygen, IV fluids, pressors, and empiric antibiotics (piperacillin-tazobactam and vancomycin) were given. Laboratory studies showed elevated white cell count (WBC 18,700/μL), procalcitonin (287 ng/mL), CRP (29 mg/dL), and ESR (113 mm/h). Chest CT described bilateral pulmonary infarcts with extensive necrosis.
A 25 mm and a 24 mm vegetations on the tricuspid valve with severe regurgitation were identified on transthoracic and transesophageal echocardiography. Bacteremia by Staphylococcus aureus sensitive to vancomycin was demonstrated.
Due to a decline in the patient's respiratory status, repeat imaging was necessary, which showed a right lung abscess and empyema. She underwent video-assisted thoracoscopic surgery (VATS) with drainage and decortication.
Significant hemoptysis prompted bronchoscopy and norepinephrine injection. Persistent blood loss with hemodynamic instability was experienced, progressing into hypovolemic shock and cardiac arrest. Resuscitation was successfully performed, followed by selective arterial embolization.
High perioperative risk prevented urgent valve replacement despite having clear indications such as severe valvular dysfunction, heart failure, large mobile vegetations, and embolization. The Angiovac system using right internal jugular access, represented a suitable option for vegetation debulking allowing 80% of the mass removal. Moderate tricuspid regurgitation persisted due to residual material on the tricuspid valve leaflet.
Conclusion:
This case is an illustration of the implications of IV drug use disorders. Infective endocarditis, septic pulmonary emboli, necrotizing abscesses, and life-threatening hemoptysis are just some of the complications that patients can experience. Multidisciplinary care is critical to achieve survival in such cases. The AngioVac system is an emerging and promising technique, offering minimally invasive options for vegetation debulking in patients with high perioperative risk.
More abstracts on this topic:
Angiography-derived FFR-Guided Coronary Artery Bypass Grafting for Patients undergoing Valve Surgery with Concomitant Coronary Artery Disease (FAVOR 4-QVAS): a Randomized Trial
Zhu Yunpeng, Guo Zhigang, Zhu Dan, Zhang Xiquan, Chen Liangwan, Redfors Bjorn, Sandner Sigrid, Gaudino Mario, Tu Shengxian, Zhao Qiang, Cheng Zhaoyun, Zhao Yuan, Zhang Wei, Han Lin, Zhang Chengxin, Yang Sumin, Ma Liang, Qiao Chenhui
The Use of Direct Oral Anticoagulants for Valvular Atrial Fibrillation in Central AustraliaSawant Sonia, Freedman Gabrielle, Terrett Sally, Garcia Ana, Khandkar Chinmay, Sivashanmugarajah Anosh, Baumann Angus