Final ID: MP74
Serratia Marcescens Aortic Valve Endocarditis in Drug Use Disorder: A Case of Catastrophic Embolic Stroke and Hemorrhagic Transformation
Abstract Body (Do not enter title and authors here): Background:
Nearly four centuries after Lazare Rivière’s first description of infective endocarditis—and over two centuries since septic embolization was recognized—a new epidemic has emerged: infective endocarditis in the era of drug use disorder.
Case report:
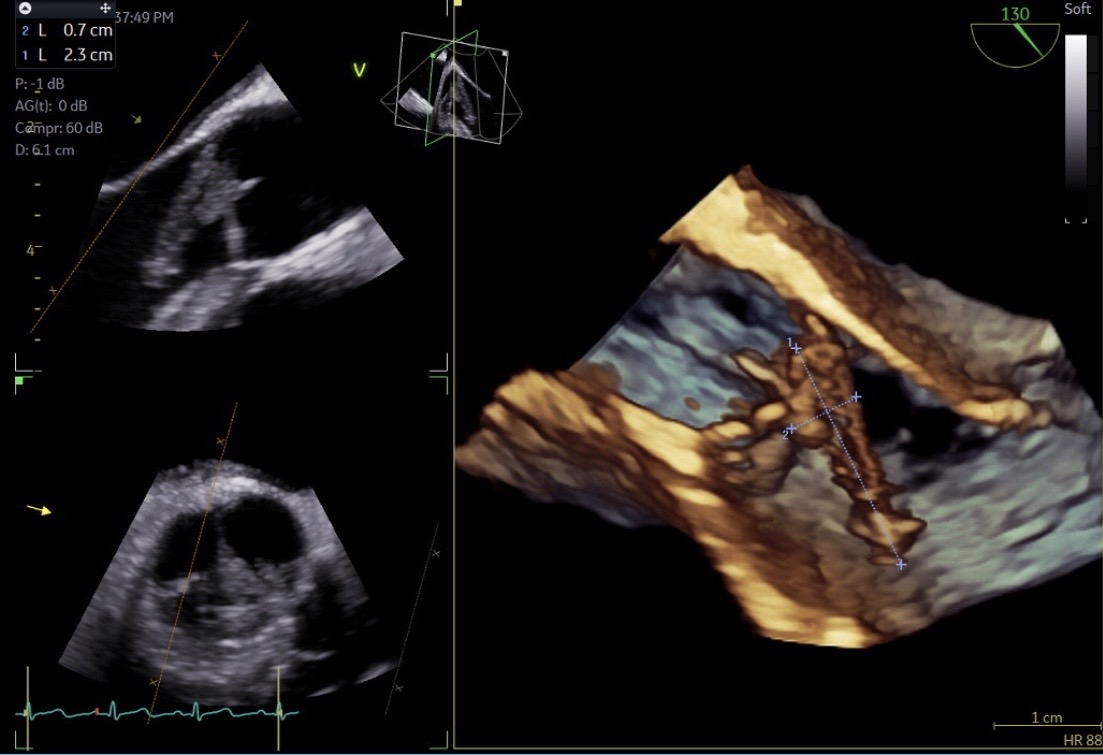
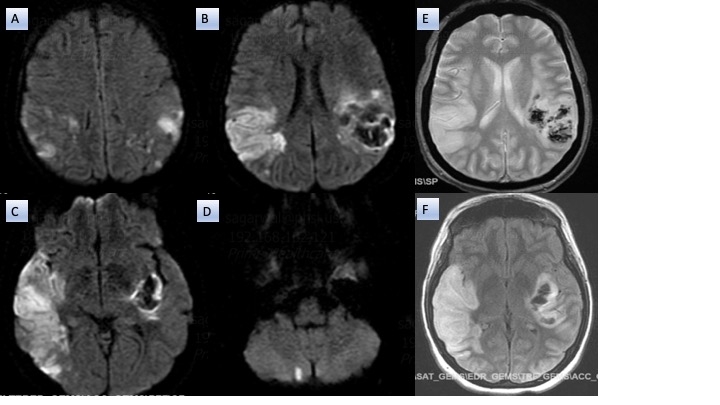
A 36-year-old woman, with drug use disorder was found unconscious with fentanyl and needles nearby. On initial evaluation, she met criteria for systemic inflammatory response syndrome: fever (T 101°F), tachycardia (HR 142 bpm), and hypotension (BP 70/43 mmHg). She was unresponsive to noxious stimuli and had a 15 cm chronic soft tissue ulcer on her right leg. Immediate management was started including endotracheal intubation, mechanical ventilation, followed by intravenous fluid resuscitation, vasopressors, and empiric Meropenem due to documented beta-lactam anaphylaxis. Laboratory studies were remarkable for elevated white blood cell count (36,700/μL), procalcitonin (17 ng/mL), CRP (13 mg/dL), ESR (110 mm/h), and lactate (7 mmol/L). Acute ischemic infarcts in bilateral frontoparietal regions and a punctate infarct in the right cerebellum were demonstrated on computerized tomography. Transthoracic and transesophageal echocardiography identified a 23 mm mobile vegetation on the aortic valve with severe regurgitation. Serratia marcescens, a gram negative fermenter bacilli susceptible to Meropenem, grew on blood and wound cultures. On hospital day 3, severe neurological deficit was observed due to hemorrhagic transformación of the left middle cerebral artery territory infarct.
Discussion:
This case underscores the complexity of infective endocarditis in the context of drug use disorders. In this case, a chronic wound represented an unconventional but lethal portal for gram-negative seeding of the aortic valve. Infective endocarditis goes beyond infection and requires a multidisciplinary approach with shared decision making. Though the presence of a large, mobile vegetation, severe valve dysfunction, and systemic embolization were indicative of urgent valve replacement; the hemorrhagic transformation of the MCA territory infarct precluded safe anticoagulation delaying aortic valve replacement. In addition, persistent severe neurological deficit required long-term supportive care such as tracheostomy and percutaneous endoscopic gastrostomy. Early recognition of drug use disorders, multidisciplinary collaboration, and integration of resources are essential to improving outcomes in this high-risk population.
Nearly four centuries after Lazare Rivière’s first description of infective endocarditis—and over two centuries since septic embolization was recognized—a new epidemic has emerged: infective endocarditis in the era of drug use disorder.
Case report:
A 36-year-old woman, with drug use disorder was found unconscious with fentanyl and needles nearby. On initial evaluation, she met criteria for systemic inflammatory response syndrome: fever (T 101°F), tachycardia (HR 142 bpm), and hypotension (BP 70/43 mmHg). She was unresponsive to noxious stimuli and had a 15 cm chronic soft tissue ulcer on her right leg. Immediate management was started including endotracheal intubation, mechanical ventilation, followed by intravenous fluid resuscitation, vasopressors, and empiric Meropenem due to documented beta-lactam anaphylaxis. Laboratory studies were remarkable for elevated white blood cell count (36,700/μL), procalcitonin (17 ng/mL), CRP (13 mg/dL), ESR (110 mm/h), and lactate (7 mmol/L). Acute ischemic infarcts in bilateral frontoparietal regions and a punctate infarct in the right cerebellum were demonstrated on computerized tomography. Transthoracic and transesophageal echocardiography identified a 23 mm mobile vegetation on the aortic valve with severe regurgitation. Serratia marcescens, a gram negative fermenter bacilli susceptible to Meropenem, grew on blood and wound cultures. On hospital day 3, severe neurological deficit was observed due to hemorrhagic transformación of the left middle cerebral artery territory infarct.
Discussion:
This case underscores the complexity of infective endocarditis in the context of drug use disorders. In this case, a chronic wound represented an unconventional but lethal portal for gram-negative seeding of the aortic valve. Infective endocarditis goes beyond infection and requires a multidisciplinary approach with shared decision making. Though the presence of a large, mobile vegetation, severe valve dysfunction, and systemic embolization were indicative of urgent valve replacement; the hemorrhagic transformation of the MCA territory infarct precluded safe anticoagulation delaying aortic valve replacement. In addition, persistent severe neurological deficit required long-term supportive care such as tracheostomy and percutaneous endoscopic gastrostomy. Early recognition of drug use disorders, multidisciplinary collaboration, and integration of resources are essential to improving outcomes in this high-risk population.
More abstracts on this topic:
3-HKA Promotes the Vascular Remodeling after Stroke by Modulating the Activation of A1/A2 Reactive Astrocytes
Chen Jun-min, Shi Guang, Yu Lulu, Shan Wei, Zhang Xiangjian, Wang Qun
3CPR Best Abstract Award: The pathogenic role of ADAMTS13 deficiency in Chronic Thromboembolic Pulmonary HypertensionWu Zhijian, Zheng X. Long, Zheng Liang