Final ID: Sa1008
Prothrombin Complex Concentrate Reduces Reoperation and Bleeding Compared to Fresh Frozen Plasma in Cardiac Surgery: A Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here): Background:
Coagulopathy after cardiac surgery is a major cause of morbidity and mortality. While prothrombin complex concentrate (PCC) is increasingly used as an alternative to fresh frozen plasma (FFP) for managing perioperative bleeding, its safety and efficacy compared to FFP remains unclear.
Research Question:
In adult patients undergoing cardiac surgery, does the use of PCC compared to FFP reduce postoperative bleeding and associated complications?
Aims:
To evaluate the safety and efficacy of PCC compared to FFP in patients undergoing cardiac surgery
Methods:
We systematically searched PubMed, Embase and the Cochrane Central from inception to May 31, 2025 for studies of adult patients (≥18 years) undergoing cardiac surgery stratified to receive either PCC or FFP. Outcomes assessed were reoperation for bleeding, chest tube drainage within 24 hours of surgery, and the incidence of stroke or transient ischemic attack (TIA). Analysis was performed using Review Manager 9.2.1. Pooled risk ratios (RR) and mean differences (MD) were calculated using a random-effects model. All statistical analyses were conducted with a 95% confidence interval, and a two-sided p-value < 0.05 was considered statistically significant. Subgroup analyses were conducted by study design (randomized controlled trials or RCTs, vs non-RCTs). Heterogeneity was assessed using τ2, χ2, and I2 statistics.
Results:
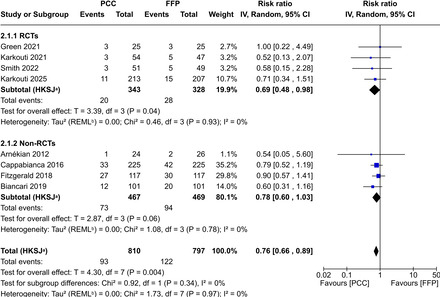
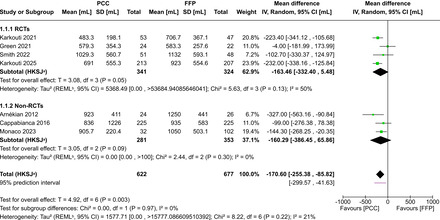
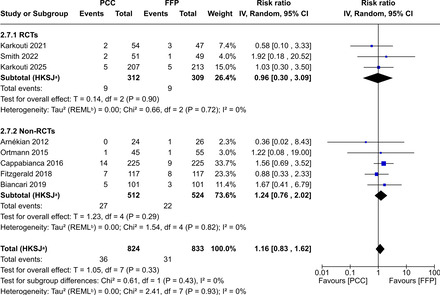
A total of 11 studies were included, of which 4 were RCTs, comprising 2,260 patients who underwent cardiac surgery. The mean age ranged from 61 to 72 years, 1586 (70.2%) were male and 959 (42.4%) received PCC. Compared to FFP, PCC use was associated with a significantly lower risk of reoperation for bleeding (RR 0.76; 95% CI, 0.66 to 0.89; P=0.004; I2=0%) and reduced chest tube drainage at 24 hours (MD −170.60 mL; 95% CI, −255.38 to −85.82; P=0.003; I2=21%). No significant difference was observed in the incidence of stroke/TIA between the two groups (RR 1.16; 95% CI, 0.83–1.62; P=0.33; I2=0%). Subgroup analyses by study design showed no significant effect modification across any outcomes (P>0.3 for all comparisons).
Conclusions:
In this meta-analysis of patients undergoing cardiac surgery, use of PCC compared with FFP was associated with a lower risk for reoperation due to bleeding and reduced postoperative chest tube output with no significant difference in the risk of stroke or TIA between groups. These findings support the use of PCC as an effective alternative to FFP in this population.
Coagulopathy after cardiac surgery is a major cause of morbidity and mortality. While prothrombin complex concentrate (PCC) is increasingly used as an alternative to fresh frozen plasma (FFP) for managing perioperative bleeding, its safety and efficacy compared to FFP remains unclear.
Research Question:
In adult patients undergoing cardiac surgery, does the use of PCC compared to FFP reduce postoperative bleeding and associated complications?
Aims:
To evaluate the safety and efficacy of PCC compared to FFP in patients undergoing cardiac surgery
Methods:
We systematically searched PubMed, Embase and the Cochrane Central from inception to May 31, 2025 for studies of adult patients (≥18 years) undergoing cardiac surgery stratified to receive either PCC or FFP. Outcomes assessed were reoperation for bleeding, chest tube drainage within 24 hours of surgery, and the incidence of stroke or transient ischemic attack (TIA). Analysis was performed using Review Manager 9.2.1. Pooled risk ratios (RR) and mean differences (MD) were calculated using a random-effects model. All statistical analyses were conducted with a 95% confidence interval, and a two-sided p-value < 0.05 was considered statistically significant. Subgroup analyses were conducted by study design (randomized controlled trials or RCTs, vs non-RCTs). Heterogeneity was assessed using τ2, χ2, and I2 statistics.
Results:
A total of 11 studies were included, of which 4 were RCTs, comprising 2,260 patients who underwent cardiac surgery. The mean age ranged from 61 to 72 years, 1586 (70.2%) were male and 959 (42.4%) received PCC. Compared to FFP, PCC use was associated with a significantly lower risk of reoperation for bleeding (RR 0.76; 95% CI, 0.66 to 0.89; P=0.004; I2=0%) and reduced chest tube drainage at 24 hours (MD −170.60 mL; 95% CI, −255.38 to −85.82; P=0.003; I2=21%). No significant difference was observed in the incidence of stroke/TIA between the two groups (RR 1.16; 95% CI, 0.83–1.62; P=0.33; I2=0%). Subgroup analyses by study design showed no significant effect modification across any outcomes (P>0.3 for all comparisons).
Conclusions:
In this meta-analysis of patients undergoing cardiac surgery, use of PCC compared with FFP was associated with a lower risk for reoperation due to bleeding and reduced postoperative chest tube output with no significant difference in the risk of stroke or TIA between groups. These findings support the use of PCC as an effective alternative to FFP in this population.
More abstracts on this topic:
Hyperoxia During Cardiopulmonary Bypass in Neonatal Congenital Heart Surgery is Associated with Worse Clinical Outcomes: A Multi-Institutional Study
Beshish Asaad, Buckley Jason, Chlebowski Meghan, Flores Saul, Goldshtrom Nimrod, Migally Karl, Mills Kimberly, Radman Monique, Reddy Chetana, Shutes Brittany, Riley Christine, Kwiatkowski David, Suguna Narasimhulu Sukumar, Mueller Dana, Amula Venugopal, Venkitachalam Raji, Joy Brian, Karki Karan, Leopold Scott, Schramm Jennifer, Capone Christine, Aydin Scott, Sznycer-taub Nathaniel, Bakar Adnan, Leong Kieran, Kulikowska Agnieszka, Mastropietro Christopher, Costello John, Jergel Andrew, Gillespie Scott, Cashen Katherine, Asfari Ahmed, Batsis Maria
Concurrent Quadruple Valve Replacement and Patent Foramen Ovale Closure for Carcinoid Heart DiseaseSchmitz Katlin, Elhadi Mohammed