Final ID: Sa1010
Hemodynamic Dance: Navigating Physiological Shifts in Ventricular Septal Defects After Myocardial Infarction
Abstract Body (Do not enter title and authors here): Description of Case:
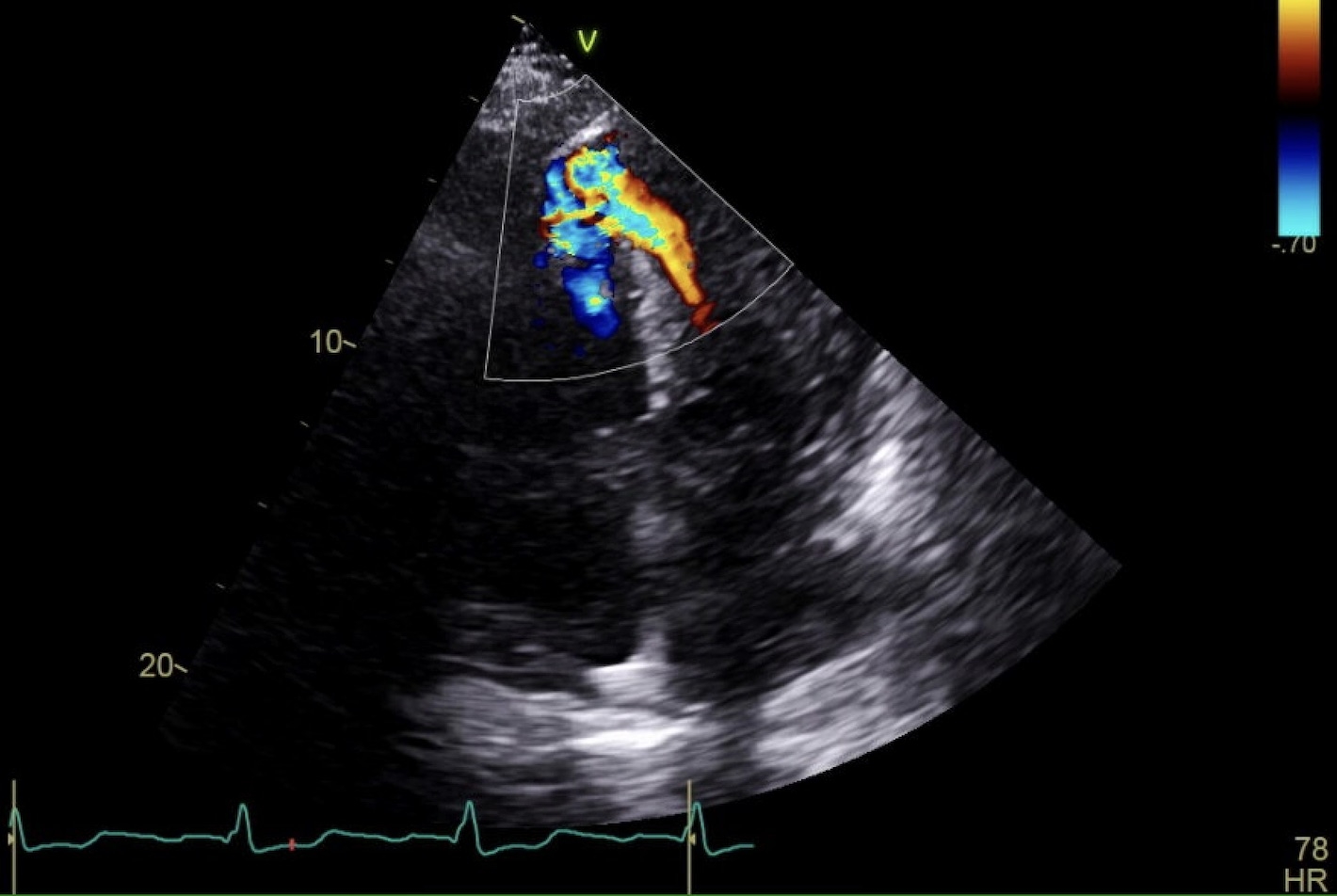
A 73-year-old male with hypertension and hyperlipidemia presented with four weeks of progressive dyspnea. He was diagnosed with an anterior STEMI and underwent left heart catheterization, receiving four stents—three in the LAD and one in D1. Despite intervention, symptoms persisted. Transthoracic echocardiogram (TTE) revealed a 1.2 cm ventricular septal defect (VSD) with left-to-right shunt and EF of 76%. Right heart catheterization showed elevated pressures: RA 18 mmHg, RV 56/20 mmHg (mean 40), PCWP 25 mmHg, and cardiac index 4.8. LAD stents were patent. Cardiothoracic surgery recommended delayed VSD repair in one month. One-week post-discharge, the patient returned with two days of worsening dyspnea and tachycardia. Exam revealed a harsh 4/6 holosystolic murmur at the lower left sternal border and bilateral leg edema. Repeat TTE showed VSD enlargement to 1.8 cm with a peak gradient of 34 mmHg and continued shunting. Inpatient VSD repair was planned. Medical management included diuresis with furosemide and afterload reduction using hydralazine and isosorbide dinitrate, titrated to blood pressure. One week later, he underwent successful VSD closure with Cardiocel patch and balloon pump support, which was subsequently removed. He was weaned to room air and discharged with outpatient follow-up.
Discussion:
Ventricular septal defects (VSDs) are life-threatening complications post-MI. Without surgical repair, mortality may reach 94% in the first month. This case highlights medical management strategies when immediate surgery is not feasible. The VSD caused left-to-right shunting, increasing right ventricular volume and pulmonary flow, ultimately straining the left atrium and ventricle. As LV function declines, vasoconstriction increases afterload and worsens shunting.
Medical stabilization focused on reducing afterload and preload. Lowering afterload redirects flow through the aorta instead of the VSD, reducing right-sided pressures. Diuretics reduce preload and stroke volume, lessening shunt impact. This approach stabilized the patient preoperatively. In refractory cases, inotropes or vasopressors may be considered. Timely surgical repair remains essential, with medical therapy serving as a critical bridge to intervention.
A 73-year-old male with hypertension and hyperlipidemia presented with four weeks of progressive dyspnea. He was diagnosed with an anterior STEMI and underwent left heart catheterization, receiving four stents—three in the LAD and one in D1. Despite intervention, symptoms persisted. Transthoracic echocardiogram (TTE) revealed a 1.2 cm ventricular septal defect (VSD) with left-to-right shunt and EF of 76%. Right heart catheterization showed elevated pressures: RA 18 mmHg, RV 56/20 mmHg (mean 40), PCWP 25 mmHg, and cardiac index 4.8. LAD stents were patent. Cardiothoracic surgery recommended delayed VSD repair in one month. One-week post-discharge, the patient returned with two days of worsening dyspnea and tachycardia. Exam revealed a harsh 4/6 holosystolic murmur at the lower left sternal border and bilateral leg edema. Repeat TTE showed VSD enlargement to 1.8 cm with a peak gradient of 34 mmHg and continued shunting. Inpatient VSD repair was planned. Medical management included diuresis with furosemide and afterload reduction using hydralazine and isosorbide dinitrate, titrated to blood pressure. One week later, he underwent successful VSD closure with Cardiocel patch and balloon pump support, which was subsequently removed. He was weaned to room air and discharged with outpatient follow-up.
Discussion:
Ventricular septal defects (VSDs) are life-threatening complications post-MI. Without surgical repair, mortality may reach 94% in the first month. This case highlights medical management strategies when immediate surgery is not feasible. The VSD caused left-to-right shunting, increasing right ventricular volume and pulmonary flow, ultimately straining the left atrium and ventricle. As LV function declines, vasoconstriction increases afterload and worsens shunting.
Medical stabilization focused on reducing afterload and preload. Lowering afterload redirects flow through the aorta instead of the VSD, reducing right-sided pressures. Diuretics reduce preload and stroke volume, lessening shunt impact. This approach stabilized the patient preoperatively. In refractory cases, inotropes or vasopressors may be considered. Timely surgical repair remains essential, with medical therapy serving as a critical bridge to intervention.
More abstracts on this topic:
OTUD6B Regulates Ventricular Chamber Maturation and Is Required for Mouse Embryonic Development
Li Yilang, Wang Wenjuan, Zambrano-carrasco Josue, Su Huabo
Simultaneous Percutaneous Ventricular Septal Closure and Mitral Valve Repair in Postinfarction Ventricular Septal Rupture and Papillary Muscle Rupture Complicated by Cardiogenic ShockGiverts Ilya, Naeem Azka, Shetty Vijay, Youdelman Benjamin