Final ID: MP2354
Association Between Site and Operator Procedural Volume and Perioperative Outcomes Following Peripheral Vascular Interventions for Chronic Limb-Threatening Ischemia
Abstract Body (Do not enter title and authors here): Background: Peripheral vascular intervention (PVI) is used to promote limb preservation in chronic limb-threatening ischemia (CLTI). Despite advancements in medical technology and risk factor management, remained stable over recent decades.
Hypothesis: Like other cardiovascular invasive procedures, higher site- and operator-level PVI volumes are associated with reduced in-hospital death, procedural complications, and technical failure.
Methods: We identified PVIs performed for CLTI in adults from 2017 to 2019 using the Medicare-linked Vascular Quality Initiative (VQI) registry. Perioperative outcomes were in-hospital death, clinical/procedural complications, and technical failure (>30% residual stenosis). We examined the association between site-level volume (per 1 additional PVI/year) and each outcome using multilevel logistic regressions. Cofounding was addressed using inverse propensity weighting based on a generalized propensity score (GPS), reflecting the likelihood of receiving PVI at a given site volume, adjusted for 16 clinical and procedural factors. Associations with operator-level PVI volume were evaluated similarly. Models included random effects for operators nested within sites to quantify outcome variations due to care delivery differences, using the intraclass correlation coefficient (ICC) and median odds ratio (MOR).
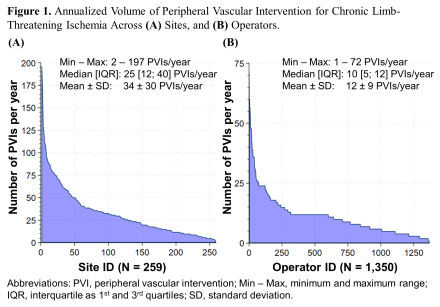
Results: We analyzed 19,439 PVIs across 259 sites by 1,350 operators (median [interquartile]: 25 [12–40] PVIs/year per site and 10 [5–13] PVIs/year per operator, Figure 1). In-hospital death occurred in 1.6% of cases, complications in 12.6%, and technical failure in 9.2%. No association was found between PVI volume at both levels for any of the outcomes (all odds ratios ~1 with 95% confidence interval narrowly ranging from 0.98 to 1.00, Table 1). Between-site differences contribute to death (ICCs<1%) but more to complications and technical failure (ICCs 10%–12%; MORs 1.78–1.88). Between-operator differences contribute to all outcomes (ICC 6%–10%; MORs 1.75–1.98).
Conclusion: Site- and operator-level PVI volumes were not associated with improved outcomes in the selected sites that subscribed to VQI. However, the meaningful variability in complications and technical failure rates across both sites and operators suggests that factors beyond volume may play a greater role in outcomes. Identifying specific site- and operator-level practices driving these differences is essential to improving PVI outcomes.
Hypothesis: Like other cardiovascular invasive procedures, higher site- and operator-level PVI volumes are associated with reduced in-hospital death, procedural complications, and technical failure.
Methods: We identified PVIs performed for CLTI in adults from 2017 to 2019 using the Medicare-linked Vascular Quality Initiative (VQI) registry. Perioperative outcomes were in-hospital death, clinical/procedural complications, and technical failure (>30% residual stenosis). We examined the association between site-level volume (per 1 additional PVI/year) and each outcome using multilevel logistic regressions. Cofounding was addressed using inverse propensity weighting based on a generalized propensity score (GPS), reflecting the likelihood of receiving PVI at a given site volume, adjusted for 16 clinical and procedural factors. Associations with operator-level PVI volume were evaluated similarly. Models included random effects for operators nested within sites to quantify outcome variations due to care delivery differences, using the intraclass correlation coefficient (ICC) and median odds ratio (MOR).
Results: We analyzed 19,439 PVIs across 259 sites by 1,350 operators (median [interquartile]: 25 [12–40] PVIs/year per site and 10 [5–13] PVIs/year per operator, Figure 1). In-hospital death occurred in 1.6% of cases, complications in 12.6%, and technical failure in 9.2%. No association was found between PVI volume at both levels for any of the outcomes (all odds ratios ~1 with 95% confidence interval narrowly ranging from 0.98 to 1.00, Table 1). Between-site differences contribute to death (ICCs<1%) but more to complications and technical failure (ICCs 10%–12%; MORs 1.78–1.88). Between-operator differences contribute to all outcomes (ICC 6%–10%; MORs 1.75–1.98).
Conclusion: Site- and operator-level PVI volumes were not associated with improved outcomes in the selected sites that subscribed to VQI. However, the meaningful variability in complications and technical failure rates across both sites and operators suggests that factors beyond volume may play a greater role in outcomes. Identifying specific site- and operator-level practices driving these differences is essential to improving PVI outcomes.
More abstracts on this topic:
Using Machine Learning Methods to Predict Adverse Events in Patients Undergoing Transcatheter Left Atrial Appendage Occlusion
Faridi Kamil, Mortazavi Bobak, Huang Sicong, Zimmerman Sarah, Friedman Daniel, Khera Rohan, Krumholz Harlan, Curtis Jeptha, Freeman James
Ability of Composite Magnetic Resonance Brain Imaging Scores to Predict Functional Outcomes in Survivors of Cardiac ArrestNguyen Thuhien, Town James, Wahlster Sarah, Johnson Nicholas, Poilvert Nicolas, Lin Victor, Ukatu Hope, Matin Nassim, Davis Arielle, Taylor Breana, Thomas Penelope, Sharma Monisha