Final ID: MP610
Patient-Level Factors Associated with Frequent, Intense, and Nocturnal Lower Extremity Pain Experience Prior Revascularization in Patients with Chronic Limb-Threatening Ischemia
Abstract Body (Do not enter title and authors here): Background: Pain is a primary symptom of chronic limb-threatening ischemia (CLTI), yet its association with patient-level factors is unclear. Identifying the key characteristics of pain in CLTI may guide personalized pain management.
Hypothesis: The frequency, intensity, and amount of nocturnal pain in CLTI correlate with depressive symptoms, ischemic severity, and other pain comorbidities.
Methods: Patients with CLTI were enrolled in the SCOPE-CLI registry at 13 U.S. and Australian centers (11/2020–04/2024). Pain severity—frequency, intensity, nocturnal pain—was derived from the Peripheral Artery Questionnaire. Patient characteristics, encompassing depressive symptoms, ischemic severity (ABI and Rutherford), pain comorbidities (duration, and back pain), were compared across pain severity groups using standardized difference (d: negligible <0.20, small 0.20—0.49, moderate 0.50—0.79, large ≥0.80). An adjusted multivariate probit model, accounting for correlations between pain severity groups, examined the probabilities of experiencing pain for each severity group by patient characteristics.
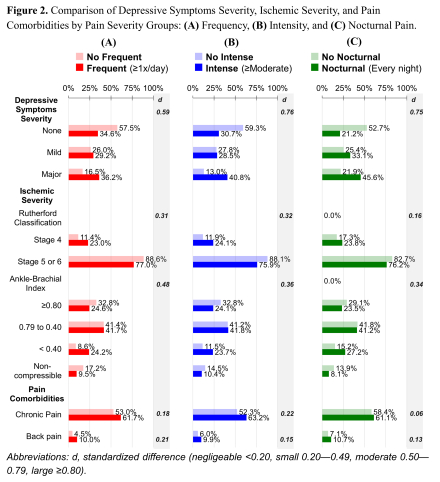
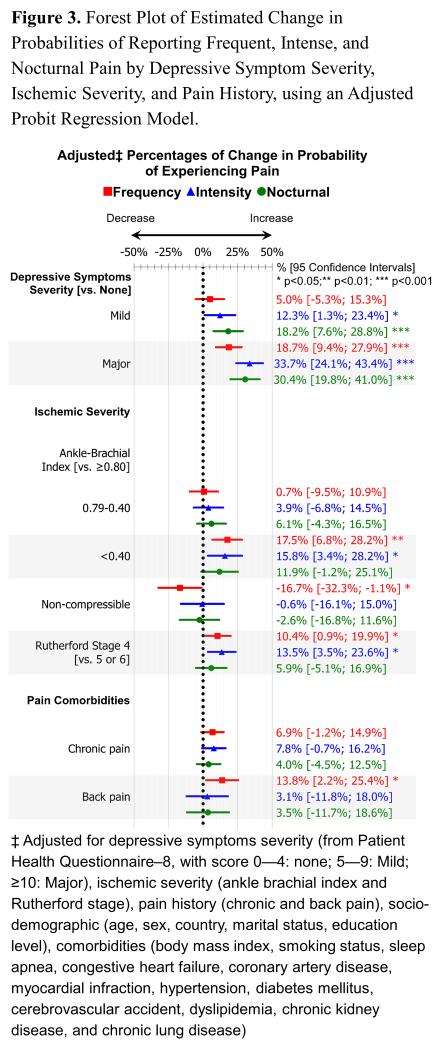
Results: Of 462 patients (mean age 68.1±10.1 years; 32.5% female), 71.4% reported frequent pain, 63.6% intense pain, and 36.4% nocturnal pain, with 20.3% reported neither (Figure 1). Most of the patients faced depressive symptoms, ankle-brachial index ≥0.40, Rutherford stage 5, and had chronic pain (≥6 months) (58.8%, 68.7%, 73.4%, and 59.4%, respectively). Those with (vs. without) frequent, intense, or nocturnal pain more likely to exhibit major depressive symptoms (36.2%, 40.8%, 45.6% vs. 16.5%, 13.0%, 22.0%, respectively; d=0.59 to 0.76), while other characteristics, including ischemic severity and pain comorbidities, showed negligeable-to-small differences (all d≤0.50, Figure 2). Probability of worsening pain increased highly with major depressive symptoms (frequent +20% [95% confidence interval: 9–28]), intense +34% [24–43], nocturnal +30% [20–41]). ABI≤0.40 and Rutherford stage 4 were modestly associated with increased probabilities of frequent and intense pain (+10.4% [0.9–19.9] to +17.5% [6.8–28.2], all p<0.001; Figure 3).
Conclusion: Nearly 80% of patients with CLTI report frequent, intense, or nocturnal pain, most of which is chronic. Pain severity, along with ischemic severity, is strongly associated with depressive symptoms. These findings highlight the need for further research into multimodal pain management strategies for CLTI.
Hypothesis: The frequency, intensity, and amount of nocturnal pain in CLTI correlate with depressive symptoms, ischemic severity, and other pain comorbidities.
Methods: Patients with CLTI were enrolled in the SCOPE-CLI registry at 13 U.S. and Australian centers (11/2020–04/2024). Pain severity—frequency, intensity, nocturnal pain—was derived from the Peripheral Artery Questionnaire. Patient characteristics, encompassing depressive symptoms, ischemic severity (ABI and Rutherford), pain comorbidities (duration, and back pain), were compared across pain severity groups using standardized difference (d: negligible <0.20, small 0.20—0.49, moderate 0.50—0.79, large ≥0.80). An adjusted multivariate probit model, accounting for correlations between pain severity groups, examined the probabilities of experiencing pain for each severity group by patient characteristics.
Results: Of 462 patients (mean age 68.1±10.1 years; 32.5% female), 71.4% reported frequent pain, 63.6% intense pain, and 36.4% nocturnal pain, with 20.3% reported neither (Figure 1). Most of the patients faced depressive symptoms, ankle-brachial index ≥0.40, Rutherford stage 5, and had chronic pain (≥6 months) (58.8%, 68.7%, 73.4%, and 59.4%, respectively). Those with (vs. without) frequent, intense, or nocturnal pain more likely to exhibit major depressive symptoms (36.2%, 40.8%, 45.6% vs. 16.5%, 13.0%, 22.0%, respectively; d=0.59 to 0.76), while other characteristics, including ischemic severity and pain comorbidities, showed negligeable-to-small differences (all d≤0.50, Figure 2). Probability of worsening pain increased highly with major depressive symptoms (frequent +20% [95% confidence interval: 9–28]), intense +34% [24–43], nocturnal +30% [20–41]). ABI≤0.40 and Rutherford stage 4 were modestly associated with increased probabilities of frequent and intense pain (+10.4% [0.9–19.9] to +17.5% [6.8–28.2], all p<0.001; Figure 3).
Conclusion: Nearly 80% of patients with CLTI report frequent, intense, or nocturnal pain, most of which is chronic. Pain severity, along with ischemic severity, is strongly associated with depressive symptoms. These findings highlight the need for further research into multimodal pain management strategies for CLTI.
More abstracts on this topic:
Association of Atrial Fibrillation with Lamotrigine in Bipolar I Disorder: An Observational Cohort Study
Kim Sodam, Welch Landon, De Los Santos Bertha, Radwanski Przemyslaw, Kim Kibum, Munger Mark
Bleeding Risks for Acute Ischemic Stroke Patients on Serotonergic Antidepressants and Anticoagulation/Dual Anti-Platelet TherapySimmonds Kent, Chavez Audrie, Ifejika Nneka