Final ID: 4347070
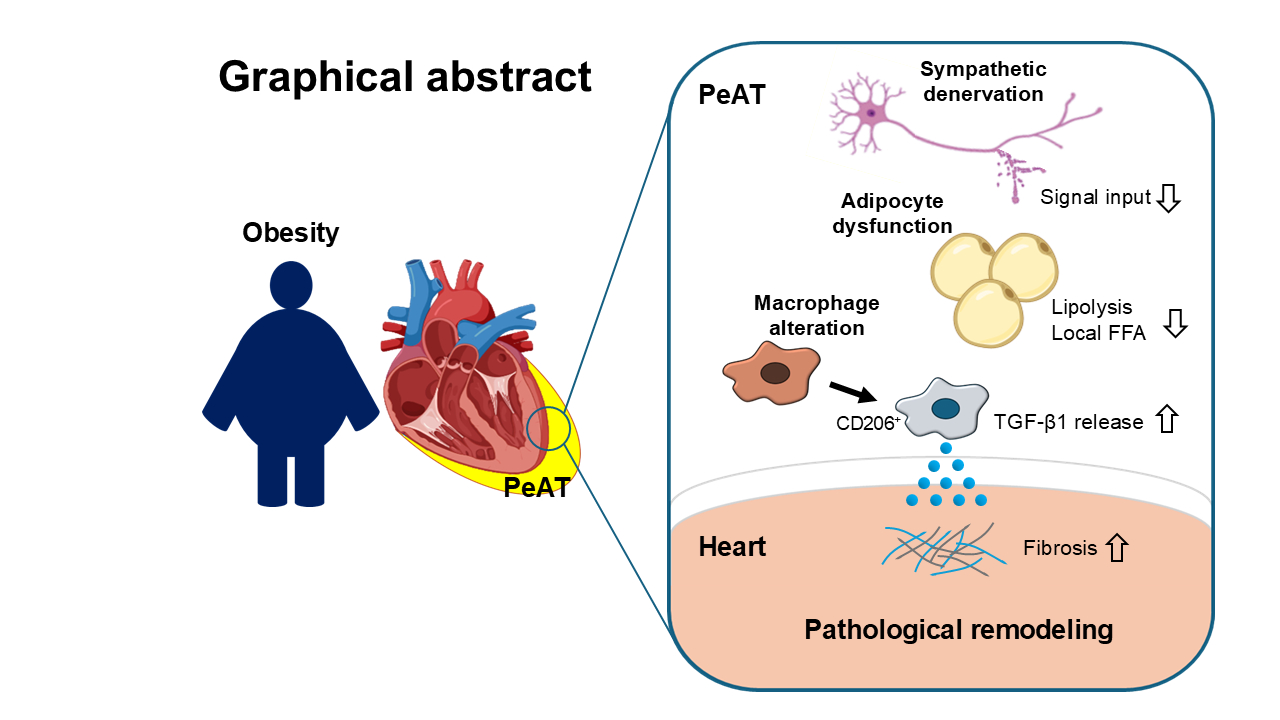
Pericardial Adipose Tissue Drives Cardiac Remodeling in Obesity via Lipolysis-Dependent Macrophage Modulation
Abstract Body (Do not enter title and authors here): Background: Obesity is a major risk factor for heart failure (HF). Recent clinical studies suggest an association between pericardial adipose tissue (PeAT) volume and HF, yet the underlying mechanisms remain elusive.
Aims: To clarify the involvement of increase in PeAT volume and development of heart failure.
Methods: Male C57BL/6 mice (8-10 weeks old) were fed a high-fat diet (HFD) for 8 weeks to induce PeAT hypertrophy. Cardiac pressure overload was induced by transverse aortic constriction (TAC) with a 26-gauge needle. Single-nucleus RNA sequencing was performed using PeAT samples from mice and HF patients.
Results: HFD feeding doubled PeAT volume in mice (15.74 ± 0.46 mg vs. 7.51 ± 0.51 mg, p<0.0001) and accelerated cardiac dysfunction (fractional shortening: 46.11 ± 2.08 vs. 56.39 ± 1.56%, p=0.012, left ventricular mass: 148.22 ± 9.92 mg vs. 108.96 ± 5.51 mg, p=0.0213), cardiomyocyte hypertrophy, and fibrosis after TAC. PeAT removal prevented the cardiac remodeling in HFD mice, whereas PeAT transplantation from obese mice to lean mice recapitulated the adverse cardiac phenotype. In HFD mice, TGF-β1 was elevated in PeAT with increased downstream SMAD2 activation in adjacent myocardium. Single-nucleus transcriptomics identified CD206+ macrophages as the primary TGF-β1 source in PeAT from both HFD mice and HF patients. Three-dimensional imaging revealed sympathetic denervation in PeAT of obese mice, accompanied by impaired β3-adrenergic receptor-mediated lipolysis signaling, resulting in reduced local free fatty acid (FFA) availability that promoted CD206+ macrophage expansion. Intrapericardial TGF-β1 neutralization ameliorated cardiac remodeling in HFD mice (fractional shortening: 39.62 ± 4.98 vs. 52.83 ± 2.47%, p=0.046, left ventricular mass: 174.0 ± 6.39 mg vs. 148.9 ± 7.94 mg, p=0.0297), and further, restoring β3-adrenergic signaling in PeAT increased local FFA levels, suppressed SMAD2 activation in the heart, and improved cardiac function after TAC (fractional shortening: 54.19 ± 1.79 vs. 59.42 ± 1.21%, p=0.034, left ventricular mass: 148.75 ± 9.05 mg vs. 105.72 ± 7.83 mg, p=0.0056).
Conclusions: These findings establish a mechanistic link between PeAT dysfunction and HF progression in obesity, highlighting PeAT as a potential therapeutic target.
Aims: To clarify the involvement of increase in PeAT volume and development of heart failure.
Methods: Male C57BL/6 mice (8-10 weeks old) were fed a high-fat diet (HFD) for 8 weeks to induce PeAT hypertrophy. Cardiac pressure overload was induced by transverse aortic constriction (TAC) with a 26-gauge needle. Single-nucleus RNA sequencing was performed using PeAT samples from mice and HF patients.
Results: HFD feeding doubled PeAT volume in mice (15.74 ± 0.46 mg vs. 7.51 ± 0.51 mg, p<0.0001) and accelerated cardiac dysfunction (fractional shortening: 46.11 ± 2.08 vs. 56.39 ± 1.56%, p=0.012, left ventricular mass: 148.22 ± 9.92 mg vs. 108.96 ± 5.51 mg, p=0.0213), cardiomyocyte hypertrophy, and fibrosis after TAC. PeAT removal prevented the cardiac remodeling in HFD mice, whereas PeAT transplantation from obese mice to lean mice recapitulated the adverse cardiac phenotype. In HFD mice, TGF-β1 was elevated in PeAT with increased downstream SMAD2 activation in adjacent myocardium. Single-nucleus transcriptomics identified CD206+ macrophages as the primary TGF-β1 source in PeAT from both HFD mice and HF patients. Three-dimensional imaging revealed sympathetic denervation in PeAT of obese mice, accompanied by impaired β3-adrenergic receptor-mediated lipolysis signaling, resulting in reduced local free fatty acid (FFA) availability that promoted CD206+ macrophage expansion. Intrapericardial TGF-β1 neutralization ameliorated cardiac remodeling in HFD mice (fractional shortening: 39.62 ± 4.98 vs. 52.83 ± 2.47%, p=0.046, left ventricular mass: 174.0 ± 6.39 mg vs. 148.9 ± 7.94 mg, p=0.0297), and further, restoring β3-adrenergic signaling in PeAT increased local FFA levels, suppressed SMAD2 activation in the heart, and improved cardiac function after TAC (fractional shortening: 54.19 ± 1.79 vs. 59.42 ± 1.21%, p=0.034, left ventricular mass: 148.75 ± 9.05 mg vs. 105.72 ± 7.83 mg, p=0.0056).
Conclusions: These findings establish a mechanistic link between PeAT dysfunction and HF progression in obesity, highlighting PeAT as a potential therapeutic target.
More abstracts on this topic:
A Randomized Placebo-Controlled Trial of Pitavastatin Calcium to Treat Combined Dyslipidemia of Obesity in Adolescents – The Pediatric Heart Network Dyslipidemia of Obesity Intervention in Teens (DO IT!) Trial
De Ferranti Sarah, Cartoski Mark, Brothers Julie, San Giovanni Christine, Zachariah Justin, Pena Sandra, Mahle William, Peterson Amy, Magge Sheela, Raghuveer Geetha, Sharma Binu, Arslanian, Md Silva, Kazlova Valiantsina, Sponseller Craig, Freemon Dandrea, Stylianou Mario, Mccrindle Brian, Mietus-snyder Michele, Urbina Elaine, Ware Adam, Teng Jessica, Trachtenberg Felicia, Russell Mark, Shah Amy
Abatacept prevents anti-PD-1-induced inflammatory heart failure development after myocardial ischemic injury in miceGergely Tamas, Buzas Edit, Neilan Tomas, Ferdinandy Peter, Varga Zoltan, Drobni Zsofia, Kovacs Tamas, Sayour Nabil, Toth Viktoria Eva, Onodi Zsofia, Kocsis Marton, Fekete Nora, Pallinger Eva