Final ID: Sa1040
CKD and Acute Myocardial Infarction-related mortality among US adults over the age of 65: Insights from CDC WONDER (1999–2020)
Abstract Body (Do not enter title and authors here):
Background
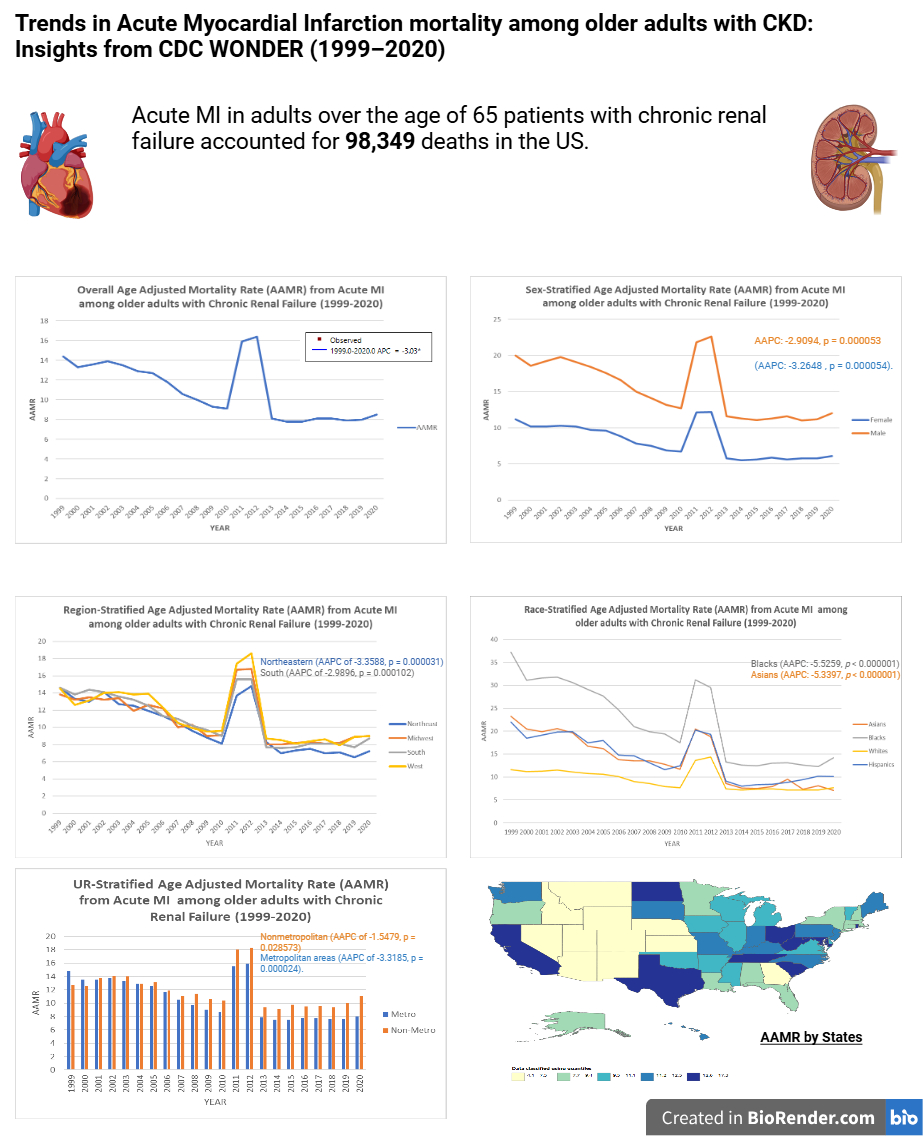
This study investigates trends in acute MI-related mortality in adults aged 65 and older with CKD, focusing on overall, geographic, and racial disparities from 1999 to 2020.
Methods
A retrospective analysis was conducted using death certificate data from the CDC WONDER database from 1999 to 2020. Age-adjusted mortality rates (AAMRs), annual percent change (APC), and average annual percentage change (AAPC) were calculated per 100,000 persons, stratified by year, sex, race/ethnicity, and geographical region.
Results
Acute MI in older (65+) patients with CKD accounted for 98349 deaths in the US. Most deaths occurred at a medical facility (57.30%). The overall AAMR for acute MI in older CKD patients decreased from 14.4 in 1999 to 8.5 in 2020, with an AAPC of -3.0286 (95 % CI: -4.2853 to -1.7555, p = 0.000083). Overall, the burden is higher in males (AAMR: 14.9) than in females (AAMR: 7.9). Over the years mortality declined in both males (AAPC: -2.9094, 95% CI: -4.0724 to -1.7323, p = 0.000053) and females (AAPC: -3.2648, 95% CI: -4.5673 to -1.9445, p = 0.000054). Racial/ethnic disparities showed the highest AAMRs in Blacks (20.8), followed by American Indians (15.4), Hispanics (13.3), Asians (12.1), and Whites (9.3). Over the years, racial stratification showed a decrease in mortality in all races. The most significant decrease was in Blacks (AAPC: -5.5259, p < 0.000001) and Asians (AAPC: -5.3397, p < 0.000001). Geographically, AAMRs ranged from 4.1 in Nevada to 17.3 in North Dakota, with the highest mortality observed in the West (AAMR: 11.1) followed by the Midwest (AAMR: 10.9). The mortality has been decreasing in all the regions with the most significant decline being in the Northeast (AAPC of -3.3588, p = 0.000031). Nonmetropolitan areas had higher AAMRs (11.8) than metropolitan areas (10.5). Overall trends show a decline in mortality for nonmetropolitan (AAPC of -1.5479, p = 0.028573) and metropolitan areas (AAPC of -3.3185, p = 0.000024).
Conclusion
The overall mortality burden from acute MI in patients above 65 with CKD has declined over the years. Males have a much higher burden than females with a decline in both sexes over the years. Racial stratification shows a higher burden on Blacks and American Indians and a decline in all races over the years. The Western states bear a significantly higher burden. Non-metropolitan areas have a higher burden. We believe these trends and disparities should be addressed via targeted policymaking.
Background
This study investigates trends in acute MI-related mortality in adults aged 65 and older with CKD, focusing on overall, geographic, and racial disparities from 1999 to 2020.
Methods
A retrospective analysis was conducted using death certificate data from the CDC WONDER database from 1999 to 2020. Age-adjusted mortality rates (AAMRs), annual percent change (APC), and average annual percentage change (AAPC) were calculated per 100,000 persons, stratified by year, sex, race/ethnicity, and geographical region.
Results
Acute MI in older (65+) patients with CKD accounted for 98349 deaths in the US. Most deaths occurred at a medical facility (57.30%). The overall AAMR for acute MI in older CKD patients decreased from 14.4 in 1999 to 8.5 in 2020, with an AAPC of -3.0286 (95 % CI: -4.2853 to -1.7555, p = 0.000083). Overall, the burden is higher in males (AAMR: 14.9) than in females (AAMR: 7.9). Over the years mortality declined in both males (AAPC: -2.9094, 95% CI: -4.0724 to -1.7323, p = 0.000053) and females (AAPC: -3.2648, 95% CI: -4.5673 to -1.9445, p = 0.000054). Racial/ethnic disparities showed the highest AAMRs in Blacks (20.8), followed by American Indians (15.4), Hispanics (13.3), Asians (12.1), and Whites (9.3). Over the years, racial stratification showed a decrease in mortality in all races. The most significant decrease was in Blacks (AAPC: -5.5259, p < 0.000001) and Asians (AAPC: -5.3397, p < 0.000001). Geographically, AAMRs ranged from 4.1 in Nevada to 17.3 in North Dakota, with the highest mortality observed in the West (AAMR: 11.1) followed by the Midwest (AAMR: 10.9). The mortality has been decreasing in all the regions with the most significant decline being in the Northeast (AAPC of -3.3588, p = 0.000031). Nonmetropolitan areas had higher AAMRs (11.8) than metropolitan areas (10.5). Overall trends show a decline in mortality for nonmetropolitan (AAPC of -1.5479, p = 0.028573) and metropolitan areas (AAPC of -3.3185, p = 0.000024).
Conclusion
The overall mortality burden from acute MI in patients above 65 with CKD has declined over the years. Males have a much higher burden than females with a decline in both sexes over the years. Racial stratification shows a higher burden on Blacks and American Indians and a decline in all races over the years. The Western states bear a significantly higher burden. Non-metropolitan areas have a higher burden. We believe these trends and disparities should be addressed via targeted policymaking.
More abstracts on this topic:
Association of Serial Seattle Angina Questionnaire Assessments with Clinical Events in Chronic Coronary Disease: Insights from the ISCHEMIA Trial
O'keefe Evan, Hochman Judith, Spertus John, Jones Philip, Cho Yoon Joo, Saxon John, Boden William, Stone Gregg, Bangalore Sripal, Reynolds Harmony, Maron David
A New Small-Molecule ErbB4 Agonist Attenuates Adverse Ventricular Remodeling After Myocardial Infarction In a Sex-Specific MannerGoovaerts Bo, Civati Celine, Feyen Eline, De Keulenaer Gilles, Segers Vincent