Final ID: MP883
In-Hospital Outcomes of Surgical Versus Transcatheter Aortic Valve Replacement in Patients with Dementia
Abstract Body (Do not enter title and authors here): Severe aortic stenosis (AS) is a progressive, life-threatening condition associated with significant morbidity and mortality. Current guidelines recommend shared decision-making regarding transcatheter aortic valve replacement (TAVR) vs. surgical aortic valve replacement (SAVR), considering valve durability and patient longevity for symptomatic patients aged 65-80. Dementia affects approximately 6.9 million Americans aged 65 and older, with nearly one-quarter between the ages of 65 and 74. Dementia is associated with increased risks of postoperative delirium, major bleeding, and prolonged hospital and ICU stays in patients undergoing cardiac surgery. However, the effect of dementia on outcomes following SAVR versus TAVR has not been well described. This study aims to address that gap by evaluating in-hospital outcomes of SAVR versus TAVR in patients with dementia in patients aged 65-80.
Using the National Inpatient Sample database, data from 2011 to 2021 was used to conduct a retrospective study of patients 18 years old or older with dementia undergoing either TAVR or SAVR, using ICD-9 and ICD-10 codes. A sub-group analysis was conducted of patients aged 65-80. Patient baseline characteristics and in-hospital outcomes were compared and adjusted for covariates to determine outcomes using a logistic regression model. Statistical significance was determined with a p-value of <0.05.sn
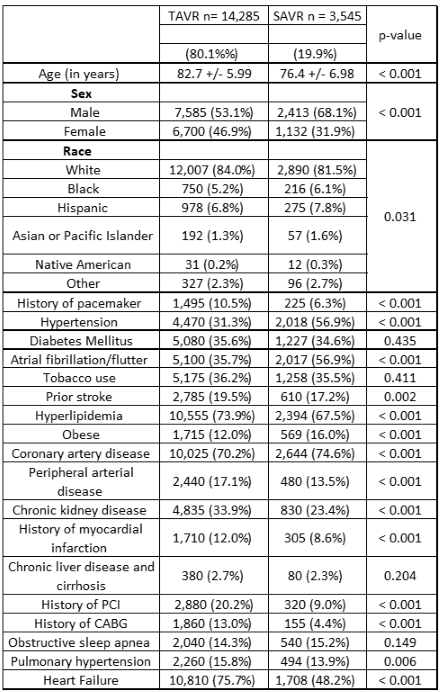
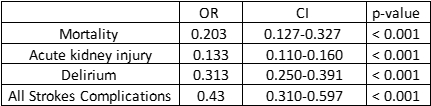
A total of 6,722 patients with dementia aged 65–80 were identified: 4,440 (80.1%) underwent TAVR and 2,282 (19.9%) underwent SAVR. In unadjusted analyses, TAVR was associated with significantly lower in-hospital mortality (0.9% vs. 3.9%), acute kidney injury (9.7% vs. 31.2%), stroke complications (2.1% vs. 6.1%), and postoperative delirium (5.3% vs. 13.8%) compared to SAVR (all p<0.001). After adjustment for covariates, TAVR remained associated with lower odds of mortality (OR 0.203; 95% CI [0.127–0.327]), acute kidney injury (OR 0.133; 95% CI [0.110–0.160]), delirium (OR 0.313; 95% CI [0.250–0.391]), and stroke complications (OR 0.430; 95% CI [0.310–0.597]) (all p<0.001).
Among patients aged 65–80 with dementia and severe AS, TAVR is associated with significantly lower in-hospital mortality, postoperative delirium, stroke complications, and acute kidney injury compared to SAVR. These findings suggest that dementia should be an important consideration in procedural selection for aortic valve replacement in this age group and support the use of TAVR in appropriate candidates.
Using the National Inpatient Sample database, data from 2011 to 2021 was used to conduct a retrospective study of patients 18 years old or older with dementia undergoing either TAVR or SAVR, using ICD-9 and ICD-10 codes. A sub-group analysis was conducted of patients aged 65-80. Patient baseline characteristics and in-hospital outcomes were compared and adjusted for covariates to determine outcomes using a logistic regression model. Statistical significance was determined with a p-value of <0.05.sn
A total of 6,722 patients with dementia aged 65–80 were identified: 4,440 (80.1%) underwent TAVR and 2,282 (19.9%) underwent SAVR. In unadjusted analyses, TAVR was associated with significantly lower in-hospital mortality (0.9% vs. 3.9%), acute kidney injury (9.7% vs. 31.2%), stroke complications (2.1% vs. 6.1%), and postoperative delirium (5.3% vs. 13.8%) compared to SAVR (all p<0.001). After adjustment for covariates, TAVR remained associated with lower odds of mortality (OR 0.203; 95% CI [0.127–0.327]), acute kidney injury (OR 0.133; 95% CI [0.110–0.160]), delirium (OR 0.313; 95% CI [0.250–0.391]), and stroke complications (OR 0.430; 95% CI [0.310–0.597]) (all p<0.001).
Among patients aged 65–80 with dementia and severe AS, TAVR is associated with significantly lower in-hospital mortality, postoperative delirium, stroke complications, and acute kidney injury compared to SAVR. These findings suggest that dementia should be an important consideration in procedural selection for aortic valve replacement in this age group and support the use of TAVR in appropriate candidates.
More abstracts on this topic:
A Meta-Analysis Comparing Same-Day Discharge to Later-Day Discharge in Transcatheter Aortic Valve Replacement
Jain Hritvik, Passey Siddhant, Jain Jyoti, Goyal Aman, Wasir Amanpreet, Ahmed Mushood, Patel Nandan, Yadav Ashish, Shah Janhvi, Mehta Aryan
Anatomic Physiological Scoring is a Comparable Predictor of Adult Congenital Operative Morbidity and MortalityLa Brenda, Taylor-fishwick Jon, Macbeth Morgan, Soohoo Megan