Final ID: MP1548
Financial Burden in Cancer Survivors with Cardiovascular Comorbidities: A Nationwide Evaluation of U.S. Healthcare Expenditures and Utilization (2016–2022)
Abstract Body (Do not enter title and authors here): Background:
Cardiovascular disease (CVD) is a major contributor to morbidity and mortality in cancer survivors, yet its cumulative economic impact remains underexplored in nationally representative populations. As both cancer survivorship and CVD prevalence rise, quantifying this dual burden is essential to inform resource allocation, optimize care, and guide policy interventions.
Hypothesis:
We evaluated healthcare expenditures and utilization among U.S. cancer survivors with and without CVD using nationally representative data.
Methods:
We conducted a retrospective cross-sectional study of the 2016–2022 Medical Expenditure Panel Survey-Household Component (MEPS-HC), including adults aged ≥18 years with diagnosis of cancer. Cardiovascular comorbidities including ischemic heart disease, myocardial infarction, heart failure, atrial fibrillation, and stroke were identified using ICD-10 codes. Annual healthcare expenditures and utilization (inpatient nights, hospital discharges, emergency room visits, office-based visits, and prescriptions) were compared between cancer survivors with and without CVD. Multivariable generalized linear models (gamma family with log link), negative binomial, and zero-inflated negative binomial regressions, adjusted for demographic, socioeconomic, and clinical confounders.
Results:
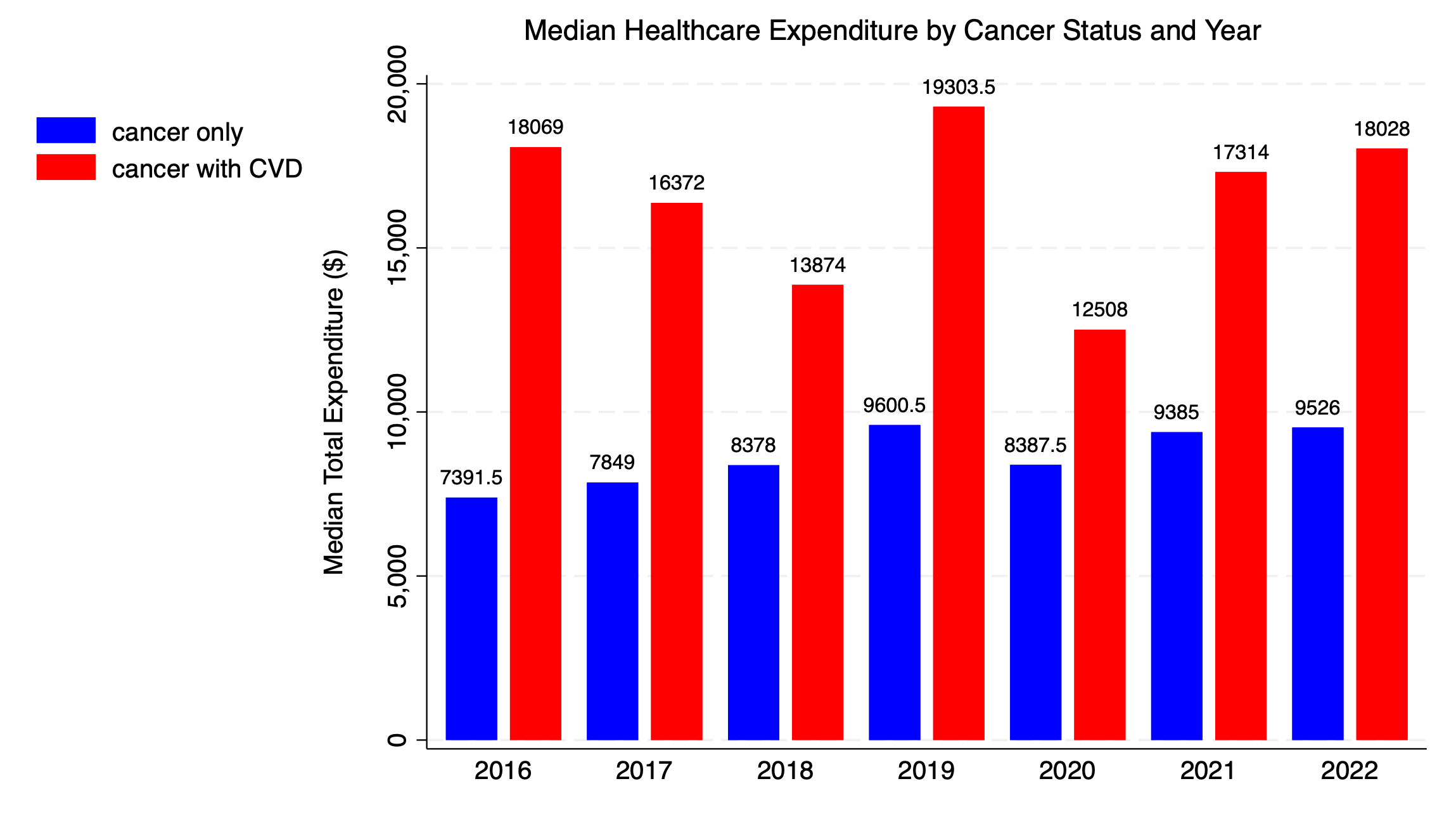
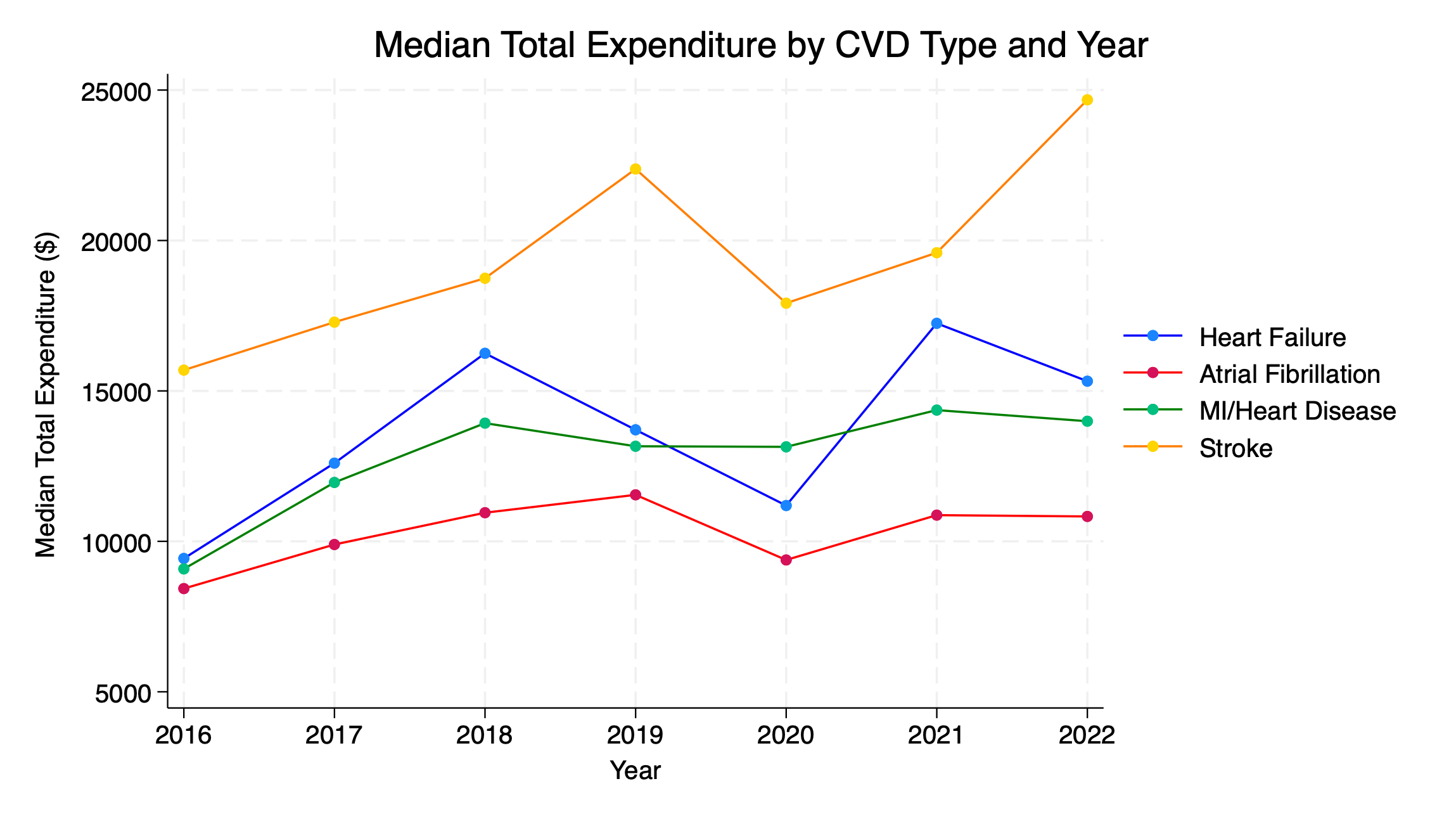
Annually, an estimated 1.19 million cancer survivors with CVD incurred 41.2% higher adjusted annual healthcare expenditures than those without CVD (marginal increase: $10,096; 95% CI: $4,394–$15,798; p=0.001). Stroke imposed the highest financial burden (+123%; +$30,518/year), followed by heart failure (+73%; +$19,000) and atrial fibrillation (+46%; +$12,393), while myocardial infarction and ischemic heart disease did not yield significant cost differences (p=0.088). Cardio-oncology patients had greater utilization: 33% more office visits (Median 14 vs 10/year; p=0.003), prescriptions (+58%), ER visits (+70%; p=0.001), and hospital discharges (+0.18/year; p=0.002). Financial hardship was linked to a 15% increase in total cost (p=0.001), regional differences accounted for 8% of expenditure variation, while Medicare coverage reduced costs up to 36% (p<0.01).
Conclusion:
Cancer survivors with CVD face significantly higher healthcare costs and utilization, particularly in the context of stroke and heart failure. These findings underscore the need for integrated cardio-oncology care and targeted policy intervention to mitigate financial toxicity and improve outcomes.
Cardiovascular disease (CVD) is a major contributor to morbidity and mortality in cancer survivors, yet its cumulative economic impact remains underexplored in nationally representative populations. As both cancer survivorship and CVD prevalence rise, quantifying this dual burden is essential to inform resource allocation, optimize care, and guide policy interventions.
Hypothesis:
We evaluated healthcare expenditures and utilization among U.S. cancer survivors with and without CVD using nationally representative data.
Methods:
We conducted a retrospective cross-sectional study of the 2016–2022 Medical Expenditure Panel Survey-Household Component (MEPS-HC), including adults aged ≥18 years with diagnosis of cancer. Cardiovascular comorbidities including ischemic heart disease, myocardial infarction, heart failure, atrial fibrillation, and stroke were identified using ICD-10 codes. Annual healthcare expenditures and utilization (inpatient nights, hospital discharges, emergency room visits, office-based visits, and prescriptions) were compared between cancer survivors with and without CVD. Multivariable generalized linear models (gamma family with log link), negative binomial, and zero-inflated negative binomial regressions, adjusted for demographic, socioeconomic, and clinical confounders.
Results:
Annually, an estimated 1.19 million cancer survivors with CVD incurred 41.2% higher adjusted annual healthcare expenditures than those without CVD (marginal increase: $10,096; 95% CI: $4,394–$15,798; p=0.001). Stroke imposed the highest financial burden (+123%; +$30,518/year), followed by heart failure (+73%; +$19,000) and atrial fibrillation (+46%; +$12,393), while myocardial infarction and ischemic heart disease did not yield significant cost differences (p=0.088). Cardio-oncology patients had greater utilization: 33% more office visits (Median 14 vs 10/year; p=0.003), prescriptions (+58%), ER visits (+70%; p=0.001), and hospital discharges (+0.18/year; p=0.002). Financial hardship was linked to a 15% increase in total cost (p=0.001), regional differences accounted for 8% of expenditure variation, while Medicare coverage reduced costs up to 36% (p<0.01).
Conclusion:
Cancer survivors with CVD face significantly higher healthcare costs and utilization, particularly in the context of stroke and heart failure. These findings underscore the need for integrated cardio-oncology care and targeted policy intervention to mitigate financial toxicity and improve outcomes.
More abstracts on this topic:
Acute Hemodynamic Effects and Synthetic Cooling Agents in “Clear” E-cigarettes Marketed in Massachusetts After the Tobacco Product Flavoring Ban
Minetti Erika, Erythropel Hanno, Keith Rachel, Davis Danielle, Zimmerman Julie, Krishnan-sarin Suchitra, Hamburg Naomi
Assessing Racial Disparities in Heart Transplant Allocations Post-2018 Policy ChangeMalkani Kabir, Zhang Ruina, Li Han, Ezema Ashley, Steitieh Diala, Purkayastha Subhanik, Kini Vinay