Final ID: MP1345
Continuing versus Discontinuing Home Beta-blockers at Admission for Possible Sepsis: A Target Trial Emulation
Abstract Body (Do not enter title and authors here): Background: Beta-blockers (BB) are commonly prescribed to patients with chronic cardiovascular disease. Despite potential benefits in septic shock, BBs are often withheld at admission for patients with sepsis. We tested whether continuation versus discontinuation of chronic BBs was associated with differences in 90-day mortality among patients admitted from the emergency department (ED) for possible sepsis.
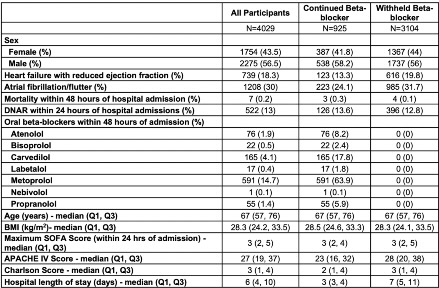
Methods: We performed a retrospective observational comparative effectiveness study under the target trial emulation framework using electronic health record data from a tertiary care medical center (Table 1). Patients ≥ 18 years on chronic BBs admitted from 1/1/2015- 12/31/2021 for suspected infection (defined by blood cultures and broad-spectrum antibiotics) were eligible. We excluded patients presenting with shock or tachycardia. The treatment variable was oral BB receipt within 48 hours of admission versus no receipt. We used Cox regression to compare time-to-death within 90 days between treatment and control groups. In secondary analyses, we used logistic regression to compare in-hospital death and negative binomial regression to compare length of stay (LOS). We performed subgroup analysis for our primary outcome for patients with heart failure with reduced ejection fraction (HFrEF). For each analysis, we constructed inverse probability of treatment weights to account for differences in sex, comorbidities, illness severity, body mass index, and presence of a do-not-resuscitate order.
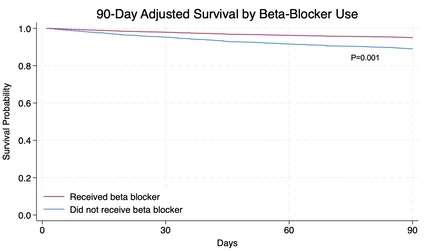
Results: We identified 4,029 patients prescribed outpatient oral BBs admitted for sepsis, with 925 patients receiving an oral BB within 48 hours. Table 2 summarizes baseline characteristics in our treatment versus control groups. In adjusted analyses, beta blockade was associated with reduced risk of all-cause mortality within 90 days of admission (HR 0.58, 95% CI: 0.42, 0.81, P=0.001, Figure) and shorter LOS (IRR 0.34, 95% CI 0.32-0.36, P < 0.001). There was no significant association between BB continuation and in-hospital mortality (OR 0.42, 95% CI: 0.16, 1.10, P=0.08), nor mortality among patients with HFrEF (HR 0.63, 95% CI: 0.30, 1.33, P=0.226).
Conclusion: At a single center, continuing oral beta blockade among a broad population of ED patients with suspected infection was associated with decreased risk of 90-day all-cause mortality and LOS. Our findings support the need for controlled studies evaluating beta-blocker continuation in patients with possible sepsis.
Methods: We performed a retrospective observational comparative effectiveness study under the target trial emulation framework using electronic health record data from a tertiary care medical center (Table 1). Patients ≥ 18 years on chronic BBs admitted from 1/1/2015- 12/31/2021 for suspected infection (defined by blood cultures and broad-spectrum antibiotics) were eligible. We excluded patients presenting with shock or tachycardia. The treatment variable was oral BB receipt within 48 hours of admission versus no receipt. We used Cox regression to compare time-to-death within 90 days between treatment and control groups. In secondary analyses, we used logistic regression to compare in-hospital death and negative binomial regression to compare length of stay (LOS). We performed subgroup analysis for our primary outcome for patients with heart failure with reduced ejection fraction (HFrEF). For each analysis, we constructed inverse probability of treatment weights to account for differences in sex, comorbidities, illness severity, body mass index, and presence of a do-not-resuscitate order.
Results: We identified 4,029 patients prescribed outpatient oral BBs admitted for sepsis, with 925 patients receiving an oral BB within 48 hours. Table 2 summarizes baseline characteristics in our treatment versus control groups. In adjusted analyses, beta blockade was associated with reduced risk of all-cause mortality within 90 days of admission (HR 0.58, 95% CI: 0.42, 0.81, P=0.001, Figure) and shorter LOS (IRR 0.34, 95% CI 0.32-0.36, P < 0.001). There was no significant association between BB continuation and in-hospital mortality (OR 0.42, 95% CI: 0.16, 1.10, P=0.08), nor mortality among patients with HFrEF (HR 0.63, 95% CI: 0.30, 1.33, P=0.226).
Conclusion: At a single center, continuing oral beta blockade among a broad population of ED patients with suspected infection was associated with decreased risk of 90-day all-cause mortality and LOS. Our findings support the need for controlled studies evaluating beta-blocker continuation in patients with possible sepsis.
More abstracts on this topic:
Disparities in Cardiovascular Multimorbidity and Mortality among Dual Medicare-Medicaid Beneficiaries: A Nationwide Cohort Study of >2 Million Patients
Lusk Jay, Kalapura Cheryl, Mentz Robert, Greene Stephen, Hammill Bradley, Mac Grory Brian, Li Fan, Xian Ying, Obrien Emily
BRASH Syndrome: A Rare But Rapidly Reversible Cause of Cardiogenic ShockImburgio Steven, Patel Palak, Alshami Abbas, Almendral Jesus, Apolito Renato, Schoenfeld Mattthew, Selan Jeffrey, Sealove Brett