Final ID: Su3041
Perinatal PM2.5 Exposure Varies by Race and Ethnicity but Does Not Mediate Disparities in Infant Cardiac Surgery Outcomes: A Causal Mediation Analysis
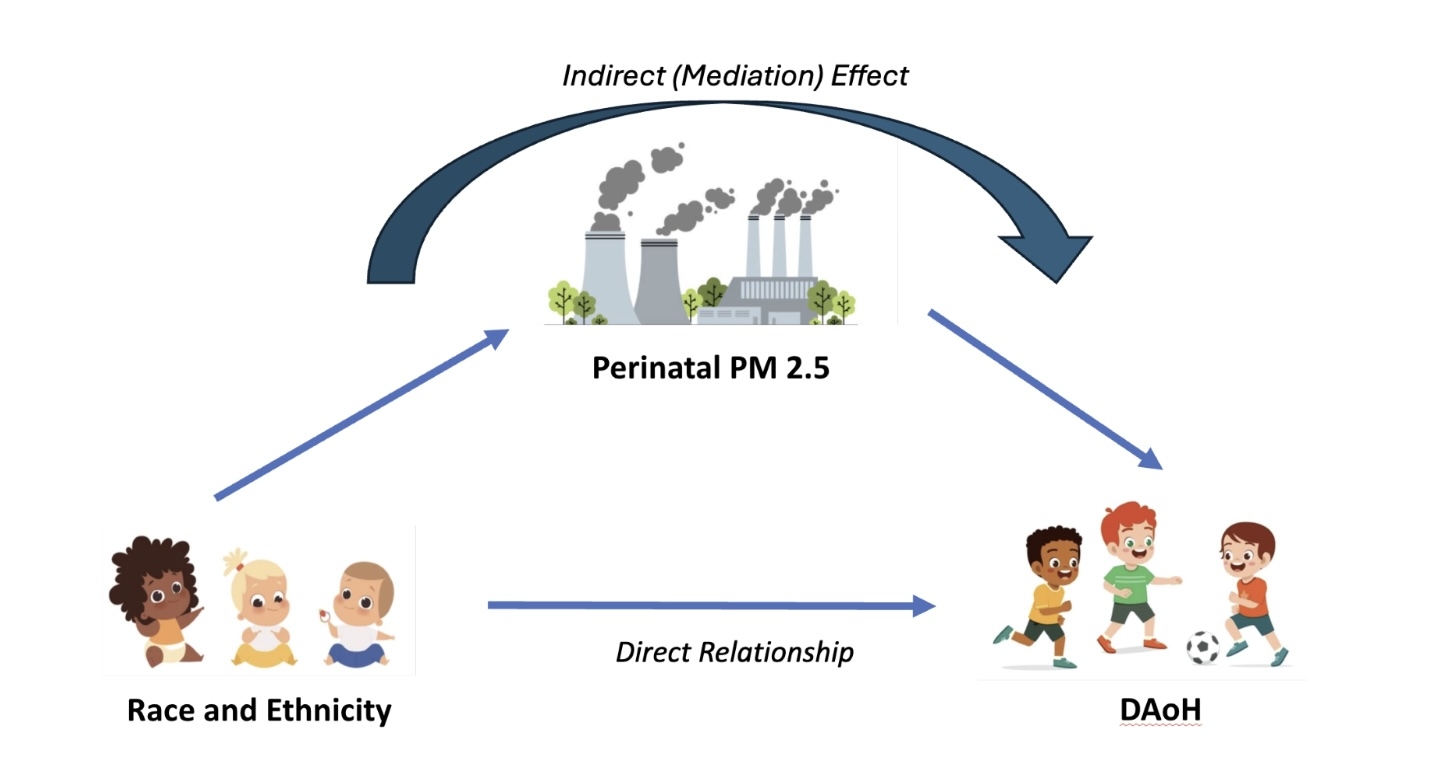
Hypothesis: Perinatal exposure to PM2.5 may be in the causal pathway between race/ethnicity and the days alive and out of healthcare (DAoH) among infants undergoing cardiac surgery (Image 1).
Methods: We linked clinical registry data from the New York State (NYS) Congenital Heart Surgery Collaborative for Longitudinal Outcomes and Utilization of Resources with Medicaid claims and census tract-level daily PM2.5 concentrations from 2006-2017. Race/ethnicity was categorized as Hispanic, Non-Hispanic (NH) Asian, NH-Black, and NH-White. Our outcome was DAoH during the first two years of life (as % of 730 days). Mediator candidates included average exposure to PM2.5 during gestational weeks 0-8, 0-35, and postnatal period ages 0-1 and 0-2 years. We applied fractional logit and linear regression for each mediator, adjusting for clinical factors and surgical center, within a causal mediation framework. Analyses were then stratified by urbanicity.
Results: Our cohort included 2,505 infants (33% Hispanic, 11% NH-Asian, 22% NH-Black, and 35% NH-White). Adjusted mean DAoH was 79.6% (95% CI 68.3-86.3) for Hispanic, 84.5% (70.3-87.3) for NH-Asian, 77.4% (66.6-86.4) for NH-Black, and 81.7% (70.0-86.3) for NH-White. In urban settings, NH-Black children experienced higher levels of PM2.5 (µg/m3) compared to NH-White children (0.44 µg/m3 [CI 0.25-0.64] at 0-35 gestational weeks, 0.44µg/m3[CI 0.27-0.61] age 0-1 year, and 0.32 µg/m3 [CI 0.16-0.48] age 0-2 years). PM2.5 exposure was not significantly associated with DAoH. Mediation analyses revealed no significant indirect effect.
Conclusion: While differences in perinatal exposure to PM2.5 were observed by race/ethnicity among infants living in urban areas, our findings suggest that this environmental factor does not mediate racial and ethnic disparities in outcomes after congenital heart surgery in NYS. This highlights the need to explore other determinants of postoperative disparities in pediatric cardiac care.
- Ramadurai, Saranya ( Mount Sinai Hospital , New York , New York , United States )
- Linder, Alexandra ( CHILDRENS HOSPITAL BOSTON , Boston , Massachusetts , United States )
- Mosca, Ralph ( NYU Medical Center , New York , New York , United States )
- Kumar, Tk ( NYU Langone Health , New York City , New York , United States )
- Devejian, Neil ( Albany Medical Center , Glenmont , New York , United States )
- Kamenir, Steven ( Albany Medical Center , Slingerlands , New York , United States )
- Alfieris, George ( University of Rochester , Rochester , New York , United States )
- Swartz, Michael ( UNIVERSITY OF ROCHESTER , Rochester , New York , United States )
- Meyer, David ( Northwell Medical Center , Uniondale , New York , United States )
- Woo, Joyce ( Lurie Children's, Northwestern U , Chicago , Illinois , United States )
- Graber, Nathan ( New York Department of Health , New York , New York , United States )
- Zhou, Eric ( Mount Sinai Hospital , New York , New York , United States )
- Sheffield, Perry ( Mount Sinai Hospital , New York , New York , United States )
- Anderson, Brett ( Icahn School of Medicine , New York , New York , United States )
- Crook, Sarah ( Mount Sinai Hospital , New York , New York , United States )
- Sanchez, Chantal ( Mount Sinai Hospital , New York , New York , United States )
- Goldstone, Andrew ( Columbia University Medical Center , New York , New York , United States )
- Billings, John ( New York University , New York , New York , United States )
- Newburger, Jane ( CHILDRENS HOSPITAL BOSTON , Boston , Massachusetts , United States )
- Jacobs, Marshall ( Johns Hopkins Medical Institution , Baltimore , Maryland , United States )
- Ebstein, Rebecca ( Cornell Medical Center , New York , New York , United States )
Meeting Info:
Session Info:
Potpourri 1: Pediatric and Congenital Cardiology
Sunday, 11/09/2025 , 11:30AM - 12:30PM
Abstract Poster Board Session
More abstracts on this topic:
Atasi Montaser, Dankar Razan, Barakat Salim, Wehbi Jad, Refaat Marwan
Cardiovascular magnetic resonance imaging estimation of diffuse myocardial and hepatic fibrosis late after tetralogy of Fallot repairMarques Lais, Rani Karur Gauri, Chaturvedi Rajiv, Friedberg Mark, Epelman Slava, Roche Susan, Wald Rachel, Ishikita Ayako, Kuruvilla Thomas Subin, Begun Isaac, Dsouza Romina, Du Plessis Jacques, Asakawa Soshun, Yuen Daren, Hanneman Kate
More abstracts from these authors:
Orie Gabrielle, Swartz Michael, Duncan Aubrey, Seltzer Laurie, Yoshitake Shuichi, Alfieris George
Impact of Social Determinants of Health on Predictive Models for Outcomes after Congenital Heart SurgeryCrook Sarah, Anderson Brett, Crook Sarah