Final ID: Mo3151
Concerning Differences in Major Amputation Trends by Hospital Medicaid Proportion, Patient Income and Race/Ethnicity
Abstract Body (Do not enter title and authors here): Introduction. Recent reports have identified a consistent reversal of decreasing trends in major lower extremity amputations, with multifactorial drivers from cardiovascular disease to societal and hospital system-based factors.
Research Question. We evaluated if major lower extremity amputation risk differs by hospital Medicaid proportion, socioeconomic status (zip code-based income), and race/ethnicity.
Methods. Using the National Inpatient Sample from 1993 to 2021, we identified inpatient admissions with procedure codes for below-knee (BKA) and above-knee (AKA) amputations. Sample-weighted, population standardized incidence rates per 100,000 people were calculated by hospital Medicaid proportions (defined as quantiles with increasing proportions), zip code-based income quartile, and race/ethnicity. Landmark analyses using multivariable logistic regressions – with inflection points identified in previous amputation incidence analyses at 2010 for BKA and 2012 for AKA – evaluated associations between amputation risk, hospital Medicaid proportion quantile, income quartile, and race/ethnicity.
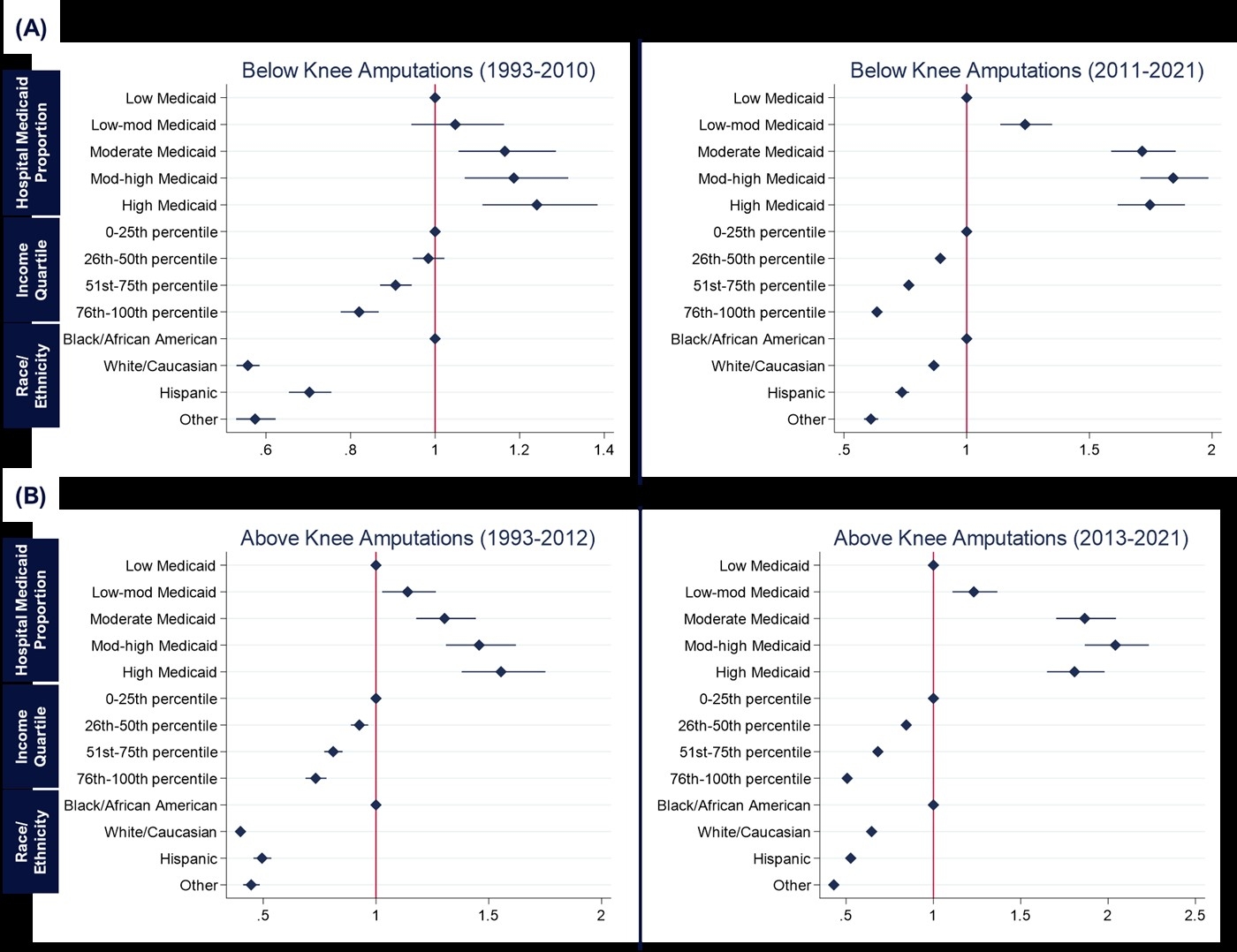
Results. In a sample of 2,769,388 admissions, 197,018 (7.1%) had BKA and 151,018 (5.5%) had AKA. Almost 50% of major amputations were performed in the highest Medicaid proportion facilities. Similarly, 38% of amputations, both AKA and BKA, were reported in the lowest income quartile. Pre-inflection points, for both AKA and BKA, we observed a clear, linearly increasing risk association between higher hospital Medicaid proportion, lower income, and being Black with amputations (Figure). Post-inflection, an elevated risk remained and was distributed relatively equally among hospitals with higher Medicaid proportions (BKA odds ratio [OR]: 1.71, 1.84, 1.75; AKA OR: 1.87, 2.04, 1.81; all p<0.001). For income, there was a widening gap with progressively greater risk in lower quartiles (BKA OR: 1.71, 1.84, 1.75; AKA OR: 1.87, 2.04, 1.81; all p<0.001).
Conclusions. Pre-inflection, high amputation risk was concentrated in extreme settings. After amputation incidence increased (i.e., post-inflection), amputation burden now spans more hospital systems and profoundly impacts lower income groups - representing changing hospital and societal risk characteristics. These findings emphasize targeting and optimizing care at high-risk hospitals and patients.
Research Question. We evaluated if major lower extremity amputation risk differs by hospital Medicaid proportion, socioeconomic status (zip code-based income), and race/ethnicity.
Methods. Using the National Inpatient Sample from 1993 to 2021, we identified inpatient admissions with procedure codes for below-knee (BKA) and above-knee (AKA) amputations. Sample-weighted, population standardized incidence rates per 100,000 people were calculated by hospital Medicaid proportions (defined as quantiles with increasing proportions), zip code-based income quartile, and race/ethnicity. Landmark analyses using multivariable logistic regressions – with inflection points identified in previous amputation incidence analyses at 2010 for BKA and 2012 for AKA – evaluated associations between amputation risk, hospital Medicaid proportion quantile, income quartile, and race/ethnicity.
Results. In a sample of 2,769,388 admissions, 197,018 (7.1%) had BKA and 151,018 (5.5%) had AKA. Almost 50% of major amputations were performed in the highest Medicaid proportion facilities. Similarly, 38% of amputations, both AKA and BKA, were reported in the lowest income quartile. Pre-inflection points, for both AKA and BKA, we observed a clear, linearly increasing risk association between higher hospital Medicaid proportion, lower income, and being Black with amputations (Figure). Post-inflection, an elevated risk remained and was distributed relatively equally among hospitals with higher Medicaid proportions (BKA odds ratio [OR]: 1.71, 1.84, 1.75; AKA OR: 1.87, 2.04, 1.81; all p<0.001). For income, there was a widening gap with progressively greater risk in lower quartiles (BKA OR: 1.71, 1.84, 1.75; AKA OR: 1.87, 2.04, 1.81; all p<0.001).
Conclusions. Pre-inflection, high amputation risk was concentrated in extreme settings. After amputation incidence increased (i.e., post-inflection), amputation burden now spans more hospital systems and profoundly impacts lower income groups - representing changing hospital and societal risk characteristics. These findings emphasize targeting and optimizing care at high-risk hospitals and patients.
More abstracts on this topic:
A Hard Start: Early, Intensive Healthcare Utilization for Children with Critical Congenital Heart Disease
Ellis Danielle, Hall Matthew, Blume Elizabeth, Wolfe Joanne, Snaman Jennifer, Berry Jay
Blood Pressure and Renal Function Outcomes After Revascularization of Renal Artery Stenosis in Patients from 3 Different Clinical SettingsMartinez Juan Luis, Clara Albert, Vazquez Susana, Galceran Isabel, Marcos Lidia, Perez Saez Maria Jose, Crespo Marta, Oliveras Anna