Final ID: MP61
Outcomes Associated with Infective Endocarditis in Cardiac Intensive Care Unit Patients
Abstract Body (Do not enter title and authors here): Introduction: Infective endocarditis (IE) is a severe intracardiac infection, often requiring intensive care unit (ICU) admission. Despite early surgical intervention, mortality remains high. Data for patients admitted to the cardiac intensive care unit (CICU) is especially limited.
Research Question: We aimed to investigate the short and long-term outcomes of patients with IE admitted to the CICU.
Methods: We conducted a retrospective cohort study of adult patients admitted to the Mayo Clinic CICU (2007-2018) with confirmed acute IE, identified via database query and manual chart review. Patients were further categorized by cardiac surgery status: performed, indicated but declined, or not indicated. Primary outcomes were all-cause mortality at 30-days and 1-year, analyzed using Kaplan-Meier and Cox proportional-hazard analysis. Models were adjusted for known predictors.
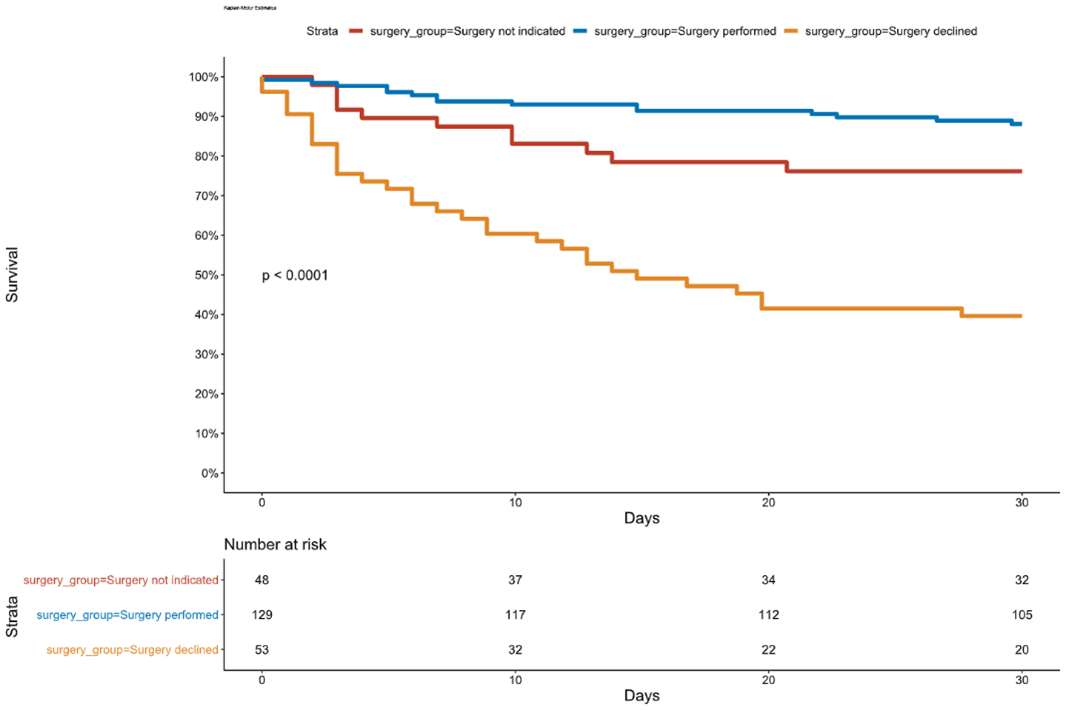
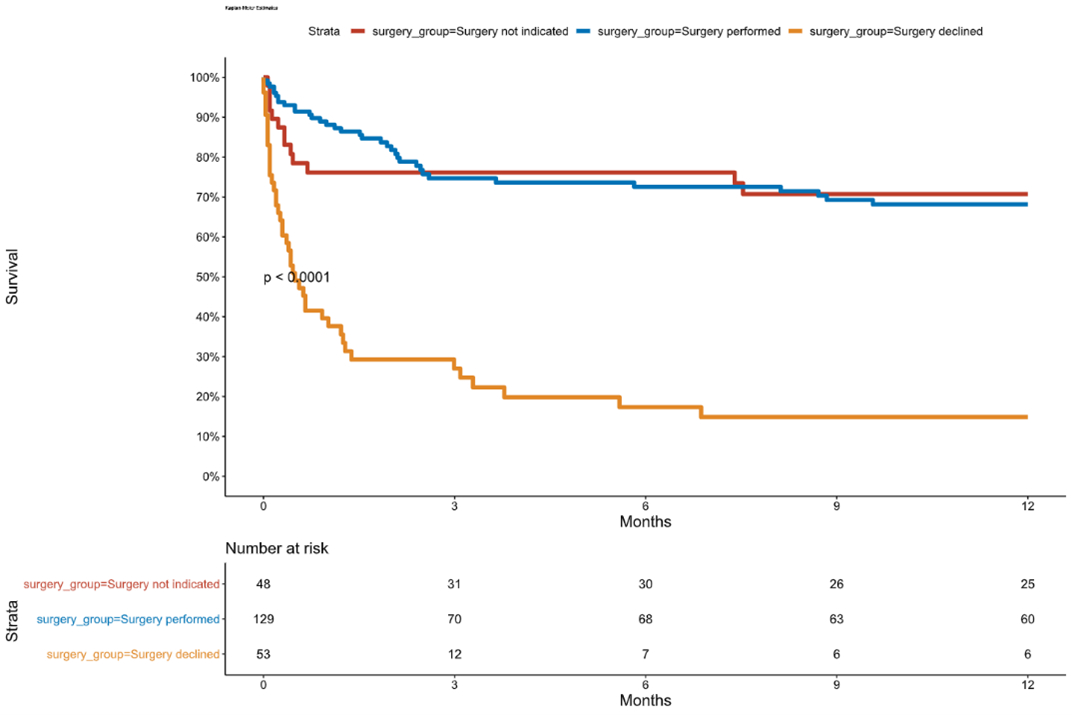
Results: Overall, 233 CICU patients met criteria for IE. Median age was 64.0 years; 49 were female. In total, 104 patients had native valve IE; 128 had prosthetic or implantable device-associated IE. Staphylococcus aureus was the most prevalent organism (42.7%) and was present in 72.4% of 30-day deaths. Cardiac surgery was indicated in 182 (78.1%) patients - 129 patients underwent surgery, while 53 declined; 48 patients did not have indications. By 30 days, 58 (24.9%) patients died; significant predictors included older age, higher illness severity scores, and greater need for critical care therapies. The 30-day mortality estimates were markedly higher for patients who declined surgery (60.4%, adj. HR 4.17, 95% CI 2.02-8.52, p <0.001), and lower for those who received surgery vs those without surgical indications (11.9% vs 23.8%, adj. HR 0.44, 95% CI 0.20-0.98, p=0.04) (Figure 1). By 1-year, 93 (39.9%) patients died, including 36 (20.5%) hospital survivors. The 1-year mortality estimates were markedly higher for patients who declined surgery (85.1%, adj. HR 5.46, 95% CI 2.87-10.39, p <0.001), but was similar for patients who received surgery to those without surgical indications (31.8% vs 29.3%, adj. HR 0.94, 95% CI 0.49-1.78, p=0.84) (Figure 2).
Conclusion: IE requiring CICU admission carries substantial mortality despite acute management. Higher severity scores, comorbidities, and intensive care interventions predict mortality. Early cardiac surgery improved short-term outcomes, but long-term mortality remains high.
Research Question: We aimed to investigate the short and long-term outcomes of patients with IE admitted to the CICU.
Methods: We conducted a retrospective cohort study of adult patients admitted to the Mayo Clinic CICU (2007-2018) with confirmed acute IE, identified via database query and manual chart review. Patients were further categorized by cardiac surgery status: performed, indicated but declined, or not indicated. Primary outcomes were all-cause mortality at 30-days and 1-year, analyzed using Kaplan-Meier and Cox proportional-hazard analysis. Models were adjusted for known predictors.
Results: Overall, 233 CICU patients met criteria for IE. Median age was 64.0 years; 49 were female. In total, 104 patients had native valve IE; 128 had prosthetic or implantable device-associated IE. Staphylococcus aureus was the most prevalent organism (42.7%) and was present in 72.4% of 30-day deaths. Cardiac surgery was indicated in 182 (78.1%) patients - 129 patients underwent surgery, while 53 declined; 48 patients did not have indications. By 30 days, 58 (24.9%) patients died; significant predictors included older age, higher illness severity scores, and greater need for critical care therapies. The 30-day mortality estimates were markedly higher for patients who declined surgery (60.4%, adj. HR 4.17, 95% CI 2.02-8.52, p <0.001), and lower for those who received surgery vs those without surgical indications (11.9% vs 23.8%, adj. HR 0.44, 95% CI 0.20-0.98, p=0.04) (Figure 1). By 1-year, 93 (39.9%) patients died, including 36 (20.5%) hospital survivors. The 1-year mortality estimates were markedly higher for patients who declined surgery (85.1%, adj. HR 5.46, 95% CI 2.87-10.39, p <0.001), but was similar for patients who received surgery to those without surgical indications (31.8% vs 29.3%, adj. HR 0.94, 95% CI 0.49-1.78, p=0.84) (Figure 2).
Conclusion: IE requiring CICU admission carries substantial mortality despite acute management. Higher severity scores, comorbidities, and intensive care interventions predict mortality. Early cardiac surgery improved short-term outcomes, but long-term mortality remains high.
More abstracts on this topic:
An Unusual Case of Listeria LVAD Infection Complicated by Intracranial Catastrophe
Zviman Julieann, Mouradjian Mallory, Rovelli Richard, Leventhal Sarah, Ananthram Manjula, Ramani Gautam, Jones Niya, Griffith Bartley, Dees Lynn, Nevin Amanda, Crowell Leigha, Soares Cullen, Amoroso Anthony
A Hemodynamic Warning Sign: Continuous Mitral Regurgitation and Normal Sinus RhythmMahi Ishani, Chowdhury Mahdi, Madan Hritik, Garg Vaani