Final ID: MP471
Outcomes of Bacteremia and Infective Endocarditis in Patients with Cardiac Implantable Electronic Devices: The Role of Device Removal
Abstract Body (Do not enter title and authors here): Background
Cardiac implantable electronic devices (CIEDs) are increasingly used to manage various cardiac conditions but are linked to a higher risk of severe infections, including bacteremia and infective endocarditis (IE). These infections often lead to longer hospital stays, higher mortality rates, and more complex clinical management. Understanding the influence of CIEDs on outcomes in these conditions is critical for optimizing treatment and informing clinical decisions, particularly regarding device removal.
Methods
We utilized the National Inpatient Sample (NIS) 2016–2019 to identify adult patients hospitalized with either a primary diagnosis of bacteremia or IE. For both cohorts, patients were stratified by the presence or absence of a CIED, identified using ICD-10 codes. The primary outcome was inpatient mortality, and the secondary outcome was length of stay (LOS). Multivariate regression analyses were performed to adjust for potential confounders.
Results
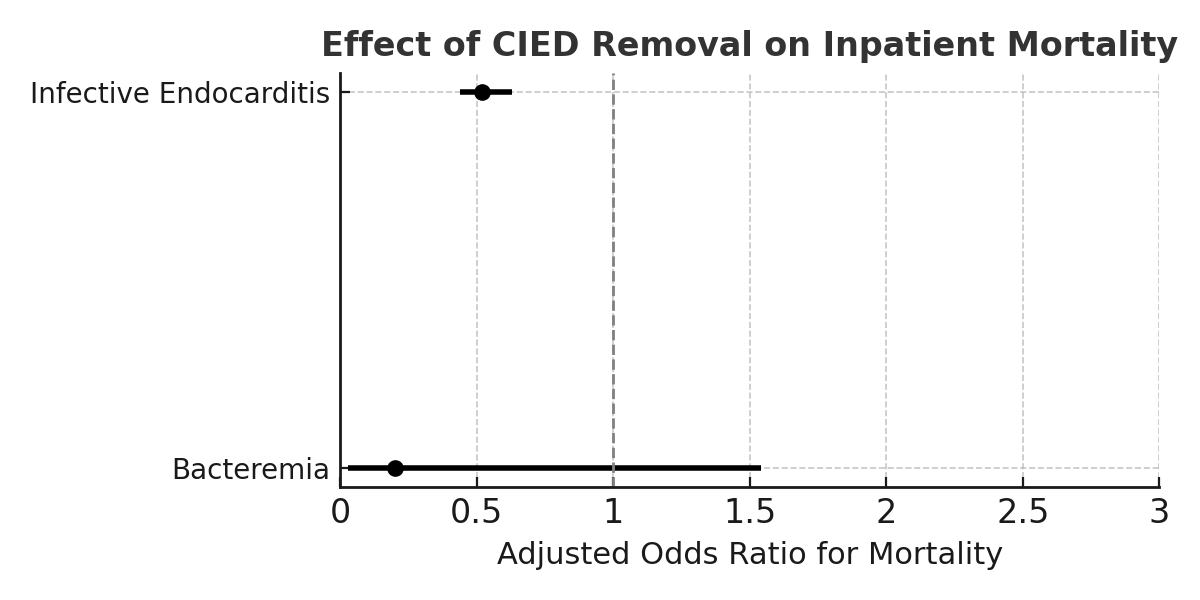
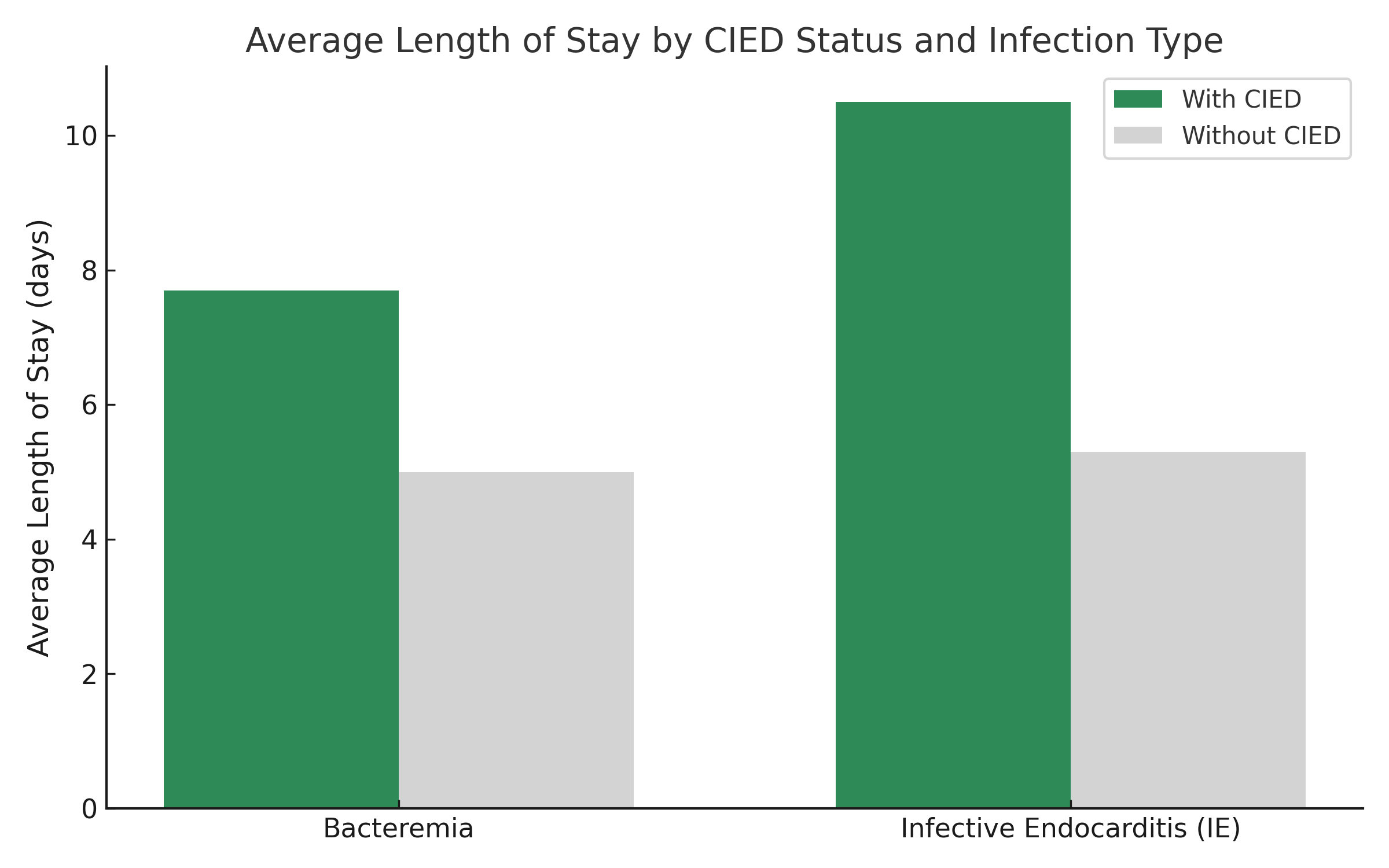
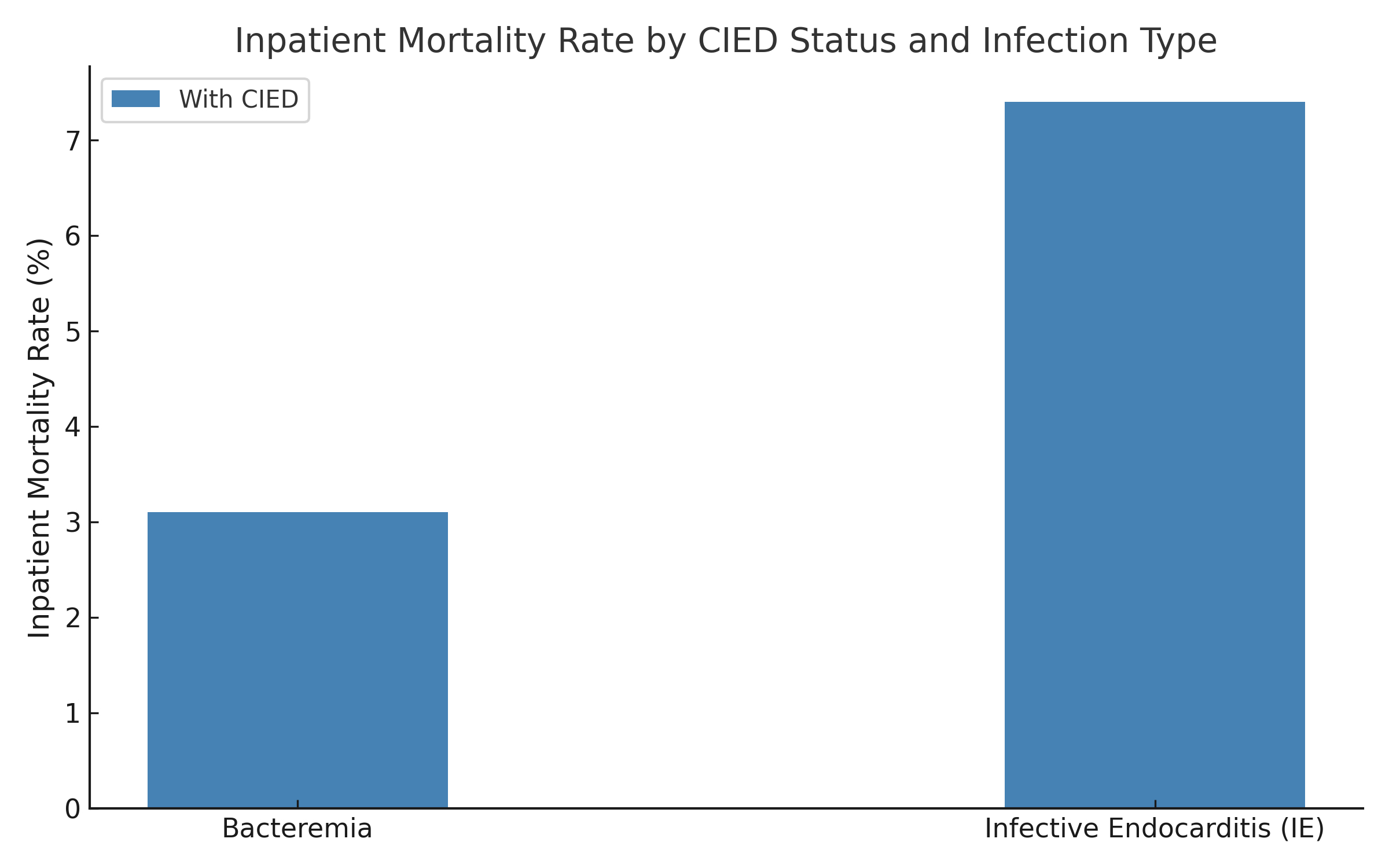
Among 671,334 patients with bacteremia, 39,875 (1%) had CIEDs and 631,459 (99%) did not. In the CIED group, 1,270 patients (3.1%) died, with an adjusted odds ratio (OR) of 0.86 (95% CI 0.75–0.98; p = 0.03) compared to the non-CIED group. CIED removal was not significantly associated with improved mortality (OR 0.2, 95% CI 0.028–1.54). The average LOS for patients with bacteremia was 5 days, but those with CIEDs had significantly longer stays (Coefficient 2.67, 95% CI 2.44–2.90).
Among 229,470 patients with IE, 15,840 (7%) had CIEDs and 213,630 (93%) did not. Mortality was significantly higher in the CIED group at 7.4% (1,184 deaths), with an OR of 2.51 (95% CI 2.17–2.91). Notably, CIED removal was associated with significantly lower mortality (OR 0.52, 95% CI 0.44–0.63). The average LOS for patients with CIEDs and IE was 10.5 days, significantly longer than for non-CIED patients (Coefficient 5.2, 95% CI 4.8–5.5).
Conclusion
Our analysis reveals a nuanced relationship between CIEDs and patient outcomes in bloodstream infections. While patients with CIEDs and bacteremia had lower inpatient mortality despite longer hospital stays, those with CIEDs and IE experienced significantly higher mortality and longer hospitalization. Importantly, CIED removal was associated with a survival benefit in IE but not in bacteremia. These findings underscore the need for infection-specific approaches to managing patients with CIEDs, particularly concerning the timing and role of device removal to improve patient outcomes.
Cardiac implantable electronic devices (CIEDs) are increasingly used to manage various cardiac conditions but are linked to a higher risk of severe infections, including bacteremia and infective endocarditis (IE). These infections often lead to longer hospital stays, higher mortality rates, and more complex clinical management. Understanding the influence of CIEDs on outcomes in these conditions is critical for optimizing treatment and informing clinical decisions, particularly regarding device removal.
Methods
We utilized the National Inpatient Sample (NIS) 2016–2019 to identify adult patients hospitalized with either a primary diagnosis of bacteremia or IE. For both cohorts, patients were stratified by the presence or absence of a CIED, identified using ICD-10 codes. The primary outcome was inpatient mortality, and the secondary outcome was length of stay (LOS). Multivariate regression analyses were performed to adjust for potential confounders.
Results
Among 671,334 patients with bacteremia, 39,875 (1%) had CIEDs and 631,459 (99%) did not. In the CIED group, 1,270 patients (3.1%) died, with an adjusted odds ratio (OR) of 0.86 (95% CI 0.75–0.98; p = 0.03) compared to the non-CIED group. CIED removal was not significantly associated with improved mortality (OR 0.2, 95% CI 0.028–1.54). The average LOS for patients with bacteremia was 5 days, but those with CIEDs had significantly longer stays (Coefficient 2.67, 95% CI 2.44–2.90).
Among 229,470 patients with IE, 15,840 (7%) had CIEDs and 213,630 (93%) did not. Mortality was significantly higher in the CIED group at 7.4% (1,184 deaths), with an OR of 2.51 (95% CI 2.17–2.91). Notably, CIED removal was associated with significantly lower mortality (OR 0.52, 95% CI 0.44–0.63). The average LOS for patients with CIEDs and IE was 10.5 days, significantly longer than for non-CIED patients (Coefficient 5.2, 95% CI 4.8–5.5).
Conclusion
Our analysis reveals a nuanced relationship between CIEDs and patient outcomes in bloodstream infections. While patients with CIEDs and bacteremia had lower inpatient mortality despite longer hospital stays, those with CIEDs and IE experienced significantly higher mortality and longer hospitalization. Importantly, CIED removal was associated with a survival benefit in IE but not in bacteremia. These findings underscore the need for infection-specific approaches to managing patients with CIEDs, particularly concerning the timing and role of device removal to improve patient outcomes.
More abstracts on this topic:
A Case of Recurrent Neurocardiogenic Syncope in a COVID-19 Patient
Naeem Nauman, Sharif Muhammad Hammad, Osama Muhammad, Takla Andrew, Arora Sahej, Khan Ghazi, Rao Mohan
A Randomized Clinical Trial Evaluating Vitamin D Normalization on Major Adverse Cardiovascular-Related Events Among Acute Coronary Syndrome Patients: The TARGET-D TrialMay Heidi, Colipi Dominique, Whiting Tyler, Muhlestein Joseph, Le Viet, Anderson Jeffrey, Babcock Daniel, Wayman Libby, Bair Tami, Knight Stacey, Knowlton Kirk, Iverson Leslie