Final ID: Su4029
Impact of New Onset Atrial Fibrillation on In-Hospital Mortality and Other Outcomes Among Patients Admitted for STEMI: A 5-Year Analysis from the National Inpatient Sample
Abstract Body (Do not enter title and authors here): Introduction: New onset atrial fibrillation (NOAF) is not a so rare condition among patients hospitalized for ST-segment elevation myocardial infarction (STEMI). However, it’s short-term prognostic value have not yet been studied using a large real-world data.
Aim: To evaluate in-hospital mortality and other clinical outcomes of this high-risk subgroup of patients using a large US real-world data.
Methods: Between January 2017 and December 2021, 855,400 STEMI patients were identified from the NIS database using ICD-10 codes. The cohort was divided into two groups: those with NOAF and those without (non-NOAF). Outcomes studied included in-hospital mortality and complications such as cardiac arrest, cardiogenic shock requiring pressors or mechanical circulatory support (MCS), acute stroke, and gastrointestinal bleed. Categorical variables were presented as percentages, and continuous variables as median ± interquartile range. Outcomes were analyzed using univariate and multivariate logistic regression to adjust for potential confounders.
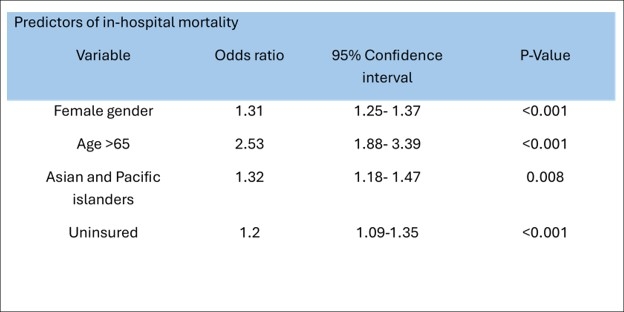
Results: Of the 855,400 STEMI patients, 51,845 (6%) developed new-onset atrial fibrillation (NOAF) during hospitalization. NOAF patients were generally older (70 vs. 63 years), more likely to be women (32.9% vs. 30%), and more often Caucasian. They also had higher rates of COPD (24.6% vs. 12.3%) and valvular diseases (13.8% vs. 8.2%) compared to non-NOAF patients. Univariate analysis showed NOAF was linked to worse outcomes. Multivariate logistic regression, adjusting for age, gender, race, insurance type and comorbidities, revealed NOAF patients had twice the risk of in-hospital mortality (OR: 2.08, CI: 1.96-2.21, P<0.001) and higher odds of complications: cardiac arrest (OR: 1.9, CI: 1.8-2.19, P<0.001), cardiogenic shock requiring MCS (OR: 2.15, CI: 1.94-2.39, P<0.001), stroke (OR: 1.36, CI: 1.19-1.56, P<0.001), and gastrointestinal bleed (OR: 1.56, CI: 1.4-1.74, P<0.001).
Conclusions: In this retrospective study, developing NOAF during index hospitalization for STEMI was associated with higher risk of in-hospital mortality and developing serious complications. Therefore, clinicians should recognize as a sign of worse prognosis and treat NOAF as soon as possible.
Aim: To evaluate in-hospital mortality and other clinical outcomes of this high-risk subgroup of patients using a large US real-world data.
Methods: Between January 2017 and December 2021, 855,400 STEMI patients were identified from the NIS database using ICD-10 codes. The cohort was divided into two groups: those with NOAF and those without (non-NOAF). Outcomes studied included in-hospital mortality and complications such as cardiac arrest, cardiogenic shock requiring pressors or mechanical circulatory support (MCS), acute stroke, and gastrointestinal bleed. Categorical variables were presented as percentages, and continuous variables as median ± interquartile range. Outcomes were analyzed using univariate and multivariate logistic regression to adjust for potential confounders.
Results: Of the 855,400 STEMI patients, 51,845 (6%) developed new-onset atrial fibrillation (NOAF) during hospitalization. NOAF patients were generally older (70 vs. 63 years), more likely to be women (32.9% vs. 30%), and more often Caucasian. They also had higher rates of COPD (24.6% vs. 12.3%) and valvular diseases (13.8% vs. 8.2%) compared to non-NOAF patients. Univariate analysis showed NOAF was linked to worse outcomes. Multivariate logistic regression, adjusting for age, gender, race, insurance type and comorbidities, revealed NOAF patients had twice the risk of in-hospital mortality (OR: 2.08, CI: 1.96-2.21, P<0.001) and higher odds of complications: cardiac arrest (OR: 1.9, CI: 1.8-2.19, P<0.001), cardiogenic shock requiring MCS (OR: 2.15, CI: 1.94-2.39, P<0.001), stroke (OR: 1.36, CI: 1.19-1.56, P<0.001), and gastrointestinal bleed (OR: 1.56, CI: 1.4-1.74, P<0.001).
Conclusions: In this retrospective study, developing NOAF during index hospitalization for STEMI was associated with higher risk of in-hospital mortality and developing serious complications. Therefore, clinicians should recognize as a sign of worse prognosis and treat NOAF as soon as possible.
More abstracts on this topic:
A Fat Chance: Paradoxical Embolic Stroke from Lipomatous Hypertrophy of the Interatrial Septum
Kalathoor Abraham
A Novel Machine Learning-based Adverse Cardiovascular Events Risk Algorithm For Cancer Patients Treated With Tyrosine Kinase InhibitorsWahi Shawn, Cross James, Mora Ruben, Im Yunju, Kwan Jennifer