Final ID: Mo4031
Assessing Coronary Artery Disease Severity: Leveraging Inflammatory Markers As a Prognostic Indicators
Abstract Body (Do not enter title and authors here): Introduction:
Cardiovascular disease continues to be the leading cause of death and a significant cause of morbidity in the United States. In recent years, there has been increased interest in the role of inflammation in predicting and modifying the risk of coronary artery disease. Of the multitude of inflammatory markers studied subsequently, two of the most easily and widely obtained is the neutrophil to lymphocyte ratio (NLR) and the monocyte to lymphocyte ratio (MLR), which can be calculated from a complete blood count with differential. Multiple retrospective studies have demonstrated that the NLR and MLR have been used to diagnose ACS, predict mortality at a year after ACS, and risk stratify patients prior to percutaneous coronary intervention.
Research Question:
Are the NLR/MLR useful tools in predicting the severity of coronary artery disease (CAD) in patients admitted to a tertiary medical center in Southern Nevada for ACS between 2021 and 2023?
Methods
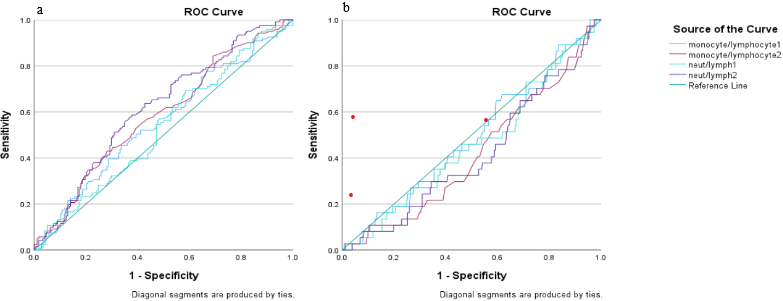
A sample of n=344 patients was used to examine the potential significance of NLR/MLR to diagnose ACS and for predicting CAD severity. Traditional diagnostic test evaluation was used for determining CAD with a ratio of NLR=3.5 + MLR=0.35 (data medians) as the cut-off value. Patient risk group status (1:low risk to 4:high risk) was used as a binary outcome to test NLR/MLR between low and high risk groups using a nonparametric MWW test of medians. Additionally, ROC analysis was used to estimate an optimized cut-off for NLR/MLR as determined by AUC.
Results:
Results demonstrate for predicting ACS using the median NLR, sensitivity=88.07; specificity=14.88; PPV=52.01; NPV=54.35), LR(+)=1.03 and LR(-)= 0.80, using the median MLR results showed sensitivity=87.28; specificity=14.11; PPV=50.84; NPV=52.17, LR(+)=1.01 and LR(-)= 0.90. Subpopulation analysis demonstrated a statistically significant difference in NLR between “high risk ACS” vs “Low Risk ACS” (p<0.001). Examination of the ROC curve for predicting the high-risk group suggested an optimized cutoff of NLR=3.7; however, AUC was only 0.617, and sensitivity and specificity were not improved compared to using the median NLR.
Conclusion
Our findings suggest that an NLR greater than 3.7 may indicate multivessel involvement or proximal/left main disease in CAD patients. However, due to its low specificity and AUC, NLR alone cannot reliably distinguish between single-vessel and multivessel CAD.
Cardiovascular disease continues to be the leading cause of death and a significant cause of morbidity in the United States. In recent years, there has been increased interest in the role of inflammation in predicting and modifying the risk of coronary artery disease. Of the multitude of inflammatory markers studied subsequently, two of the most easily and widely obtained is the neutrophil to lymphocyte ratio (NLR) and the monocyte to lymphocyte ratio (MLR), which can be calculated from a complete blood count with differential. Multiple retrospective studies have demonstrated that the NLR and MLR have been used to diagnose ACS, predict mortality at a year after ACS, and risk stratify patients prior to percutaneous coronary intervention.
Research Question:
Are the NLR/MLR useful tools in predicting the severity of coronary artery disease (CAD) in patients admitted to a tertiary medical center in Southern Nevada for ACS between 2021 and 2023?
Methods
A sample of n=344 patients was used to examine the potential significance of NLR/MLR to diagnose ACS and for predicting CAD severity. Traditional diagnostic test evaluation was used for determining CAD with a ratio of NLR=3.5 + MLR=0.35 (data medians) as the cut-off value. Patient risk group status (1:low risk to 4:high risk) was used as a binary outcome to test NLR/MLR between low and high risk groups using a nonparametric MWW test of medians. Additionally, ROC analysis was used to estimate an optimized cut-off for NLR/MLR as determined by AUC.
Results:
Results demonstrate for predicting ACS using the median NLR, sensitivity=88.07; specificity=14.88; PPV=52.01; NPV=54.35), LR(+)=1.03 and LR(-)= 0.80, using the median MLR results showed sensitivity=87.28; specificity=14.11; PPV=50.84; NPV=52.17, LR(+)=1.01 and LR(-)= 0.90. Subpopulation analysis demonstrated a statistically significant difference in NLR between “high risk ACS” vs “Low Risk ACS” (p<0.001). Examination of the ROC curve for predicting the high-risk group suggested an optimized cutoff of NLR=3.7; however, AUC was only 0.617, and sensitivity and specificity were not improved compared to using the median NLR.
Conclusion
Our findings suggest that an NLR greater than 3.7 may indicate multivessel involvement or proximal/left main disease in CAD patients. However, due to its low specificity and AUC, NLR alone cannot reliably distinguish between single-vessel and multivessel CAD.
More abstracts on this topic:
84 Immune checkpoint profiling in major aortic diseases leads to identification of potential roles of CD155-CD206 pathway in suppressing inflammation and immune responses
Shao Ying, Saaoud Fatma, Xu Keman, Lu Yifan, Jiang Xiaohua, Wang Hong, Yang Xiaofeng
12-lead electrocardiograms predict adverse cardiovascular outcomes of emergency department patientsHaimovich Julian, Kolossvary Marton, Alam Ridwan, Padros I Valls Raimon, Lu Michael, Aguirre Aaron