Final ID: 4147597
Venoarterial Extracorporeal Membrane Oxygenation With and Without Left Ventricular Unloading in Patients With Cardiac Arrest
Abstract Body (Do not enter title and authors here): Background: Extracorporeal cardiopulmonary resuscitation (ECPR) using venoarterial extracorporeal membrane oxygenation (VA-ECMO) is a promising strategy for refractory cardiac arrest. However, the role of left ventricular (LV) unloading during ECPR remains uncertain.
Methods: We queried the United States National Inpatient Sample (2016-2021) to identify adult patients with out-of-hospital (OHCA) and in-hospital cardiac arrest (IHCA) who received ECPR. Patients were stratified based on the use of either VA-ECMO only or VA-ECMO with intra-aortic balloon pump (IABP) or VA-ECMO with Impella (ECPELLA) for ventricular unloading. Multivariable logistic regression was used to compare in-hospital outcomes between the groups.
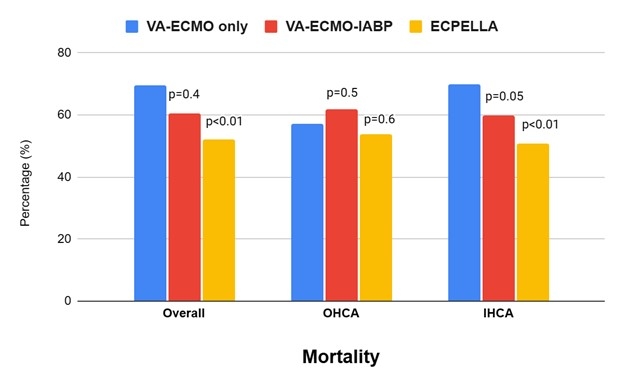
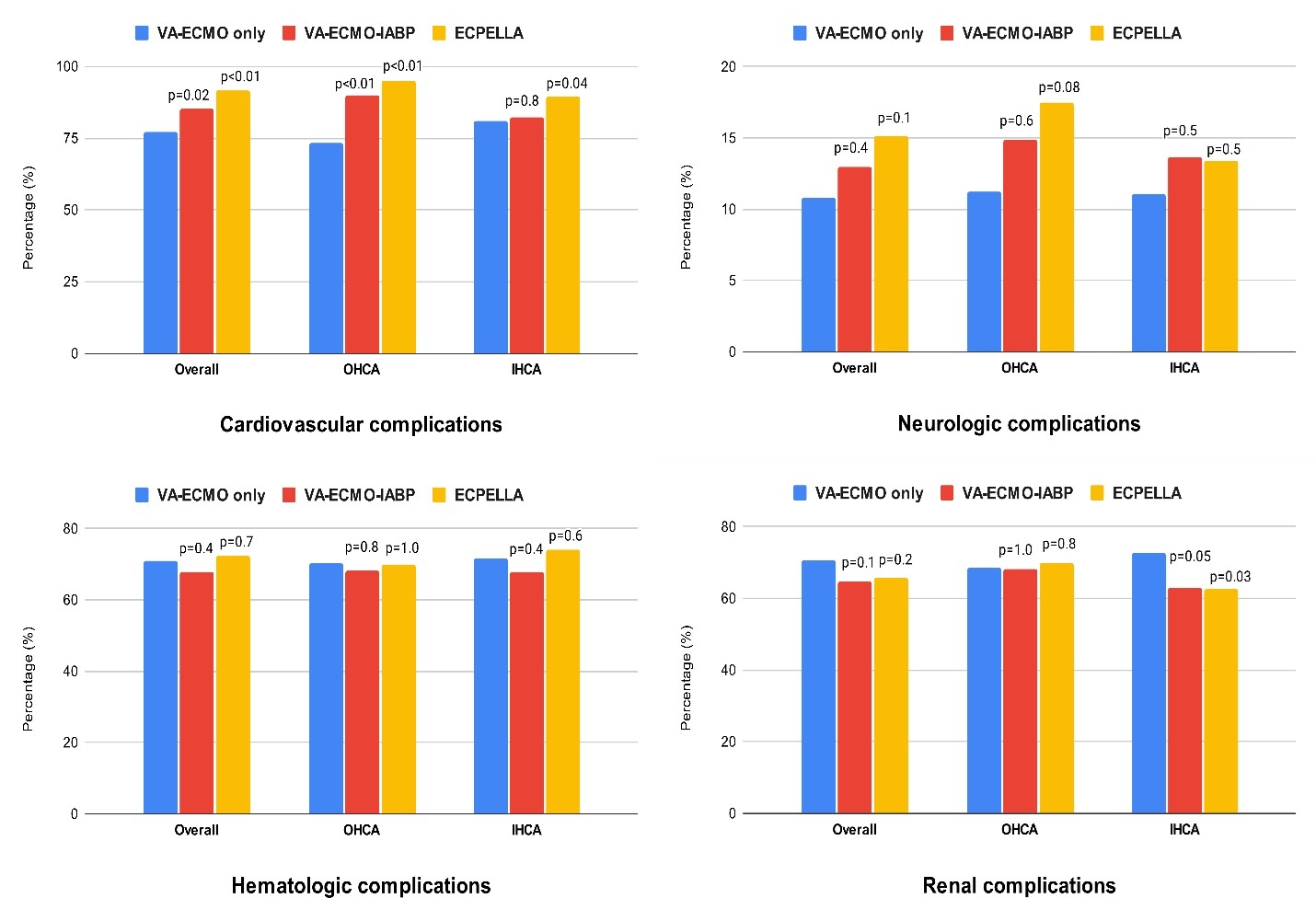
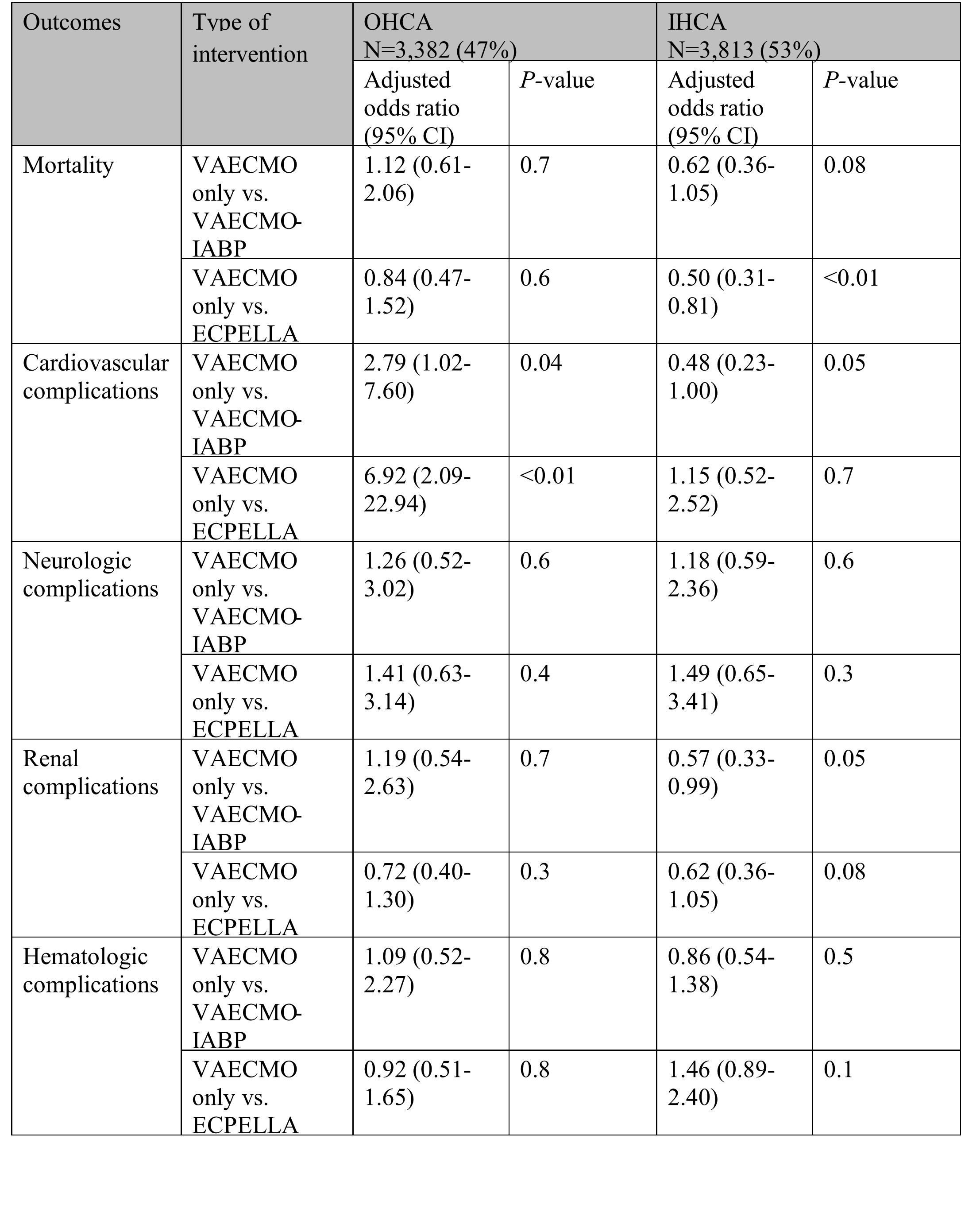
Results: Among 6,915 patients receiving ECPR, VA-ECMO alone was used in 5,145 (74.4%), VA-ECMO-IABP in 809 (11.7%), and ECPELLA in 961 (13.9%). The LV unloading groups more frequently presented with ventricular tachycardia/fibrillation (61.1% and 72.4% vs. 43.9%, both p<0.01), while the VA-ECMO only group more often presented with pulseless electrical activity/asystole (56.1% vs. 38.9% and 27.6%, both p<0.01). In IHCA patients, ECPELLA was associated with 50% lower odds of in-hospital mortality compared to VA-ECMO alone (adjusted odds ratio [aOR] 0.50, 95% CI 0.31-0.81, p<0.01). No significant difference was found in OHCA patients. VA-ECMO-IABP was not associated with a mortality benefit vs. VA-ECMO alone in either OHCA or IHCA (Figure 1). Cardiovascular complications were significantly higher in both LV unloading groups compared to the VA-ECMO only group in OHCA subgroup (90% and 95% vs. 73.3%, both p<0.01) while IHCA subgroup only showed higher significant rates in ECPELLA compared to VA-ECMO alone (89.3% vs. 81%, p=0.04) (Figure 2). After adjustment for potential confounders, VA-ECMO-IABP (aOR 2.79, 95% CI 1.02-7.60, p=0.04) and ECPELLA (aOR 6.92, 95% CI 2.09-22.94, p<0.01) were associated with significantly higher odds of cardiovascular complications compared to VA-ECMO alone among OHCA patients, but not among IHCA patient. There were no statistically significant differences in neurologic, renal, and hematologic complications between the three groups in either OHCA or IHCA patients (Figure 3).
Conclusion: In this nationwide study, LV unloading with ECPELLA was associated with improved survival in IHCA patients but not in OHCA patients compared to VA-ECMO alone. The addition of IABP to VA-ECMO was not associated with a mortality benefit.
Methods: We queried the United States National Inpatient Sample (2016-2021) to identify adult patients with out-of-hospital (OHCA) and in-hospital cardiac arrest (IHCA) who received ECPR. Patients were stratified based on the use of either VA-ECMO only or VA-ECMO with intra-aortic balloon pump (IABP) or VA-ECMO with Impella (ECPELLA) for ventricular unloading. Multivariable logistic regression was used to compare in-hospital outcomes between the groups.
Results: Among 6,915 patients receiving ECPR, VA-ECMO alone was used in 5,145 (74.4%), VA-ECMO-IABP in 809 (11.7%), and ECPELLA in 961 (13.9%). The LV unloading groups more frequently presented with ventricular tachycardia/fibrillation (61.1% and 72.4% vs. 43.9%, both p<0.01), while the VA-ECMO only group more often presented with pulseless electrical activity/asystole (56.1% vs. 38.9% and 27.6%, both p<0.01). In IHCA patients, ECPELLA was associated with 50% lower odds of in-hospital mortality compared to VA-ECMO alone (adjusted odds ratio [aOR] 0.50, 95% CI 0.31-0.81, p<0.01). No significant difference was found in OHCA patients. VA-ECMO-IABP was not associated with a mortality benefit vs. VA-ECMO alone in either OHCA or IHCA (Figure 1). Cardiovascular complications were significantly higher in both LV unloading groups compared to the VA-ECMO only group in OHCA subgroup (90% and 95% vs. 73.3%, both p<0.01) while IHCA subgroup only showed higher significant rates in ECPELLA compared to VA-ECMO alone (89.3% vs. 81%, p=0.04) (Figure 2). After adjustment for potential confounders, VA-ECMO-IABP (aOR 2.79, 95% CI 1.02-7.60, p=0.04) and ECPELLA (aOR 6.92, 95% CI 2.09-22.94, p<0.01) were associated with significantly higher odds of cardiovascular complications compared to VA-ECMO alone among OHCA patients, but not among IHCA patient. There were no statistically significant differences in neurologic, renal, and hematologic complications between the three groups in either OHCA or IHCA patients (Figure 3).
Conclusion: In this nationwide study, LV unloading with ECPELLA was associated with improved survival in IHCA patients but not in OHCA patients compared to VA-ECMO alone. The addition of IABP to VA-ECMO was not associated with a mortality benefit.
More abstracts on this topic:
A Predictive Score for In-Transit Cardiac Arrest in Trauma Patients: Development and Validation Using a National Registry
Nishida Tsubasa, Nishikimi Mitsuaki, Namba Takeshi, Ohshimo Shinichiro, Shime Nobuaki
Imaging-Guided Retrieval of a Migrated Coil from the Right Atrium: A Multimodal Endovascular ApproachBharaj Inderjeet Singh, Thwe Ei Ei, Padda Inderbir, Pan Hao, Loli Akil, Prutzman David, Alkhatib Basil, Sethi Yashendra