Final ID: Su4168
Catastrophic Bioprosthetic Aortic Valve Thrombosis: An Unappreciated Complication of Veno-Arterial Extracorporeal Membrane Oxygenation Support in Cardiogenic Shock
Abstract Body (Do not enter title and authors here): Description of Case
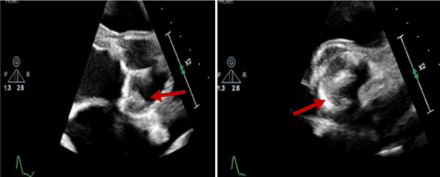
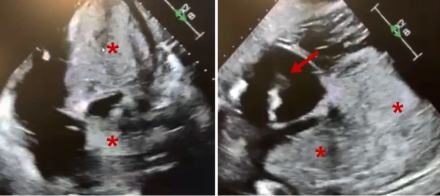
A 56-year-old male with a history of cardiac sarcoidosis with biventricular systolic heart failure (HF) and a bioprosthetic aortic valve presented with acute decompensated HF. Progressive cardiogenic shock and hemodynamic instability ensued, requiring urgent bedside placement of an intra-aortic balloon pump (IABP) which provided only marginal hemodynamic support. After extensive multidisciplinary discussion, emergent cannulation for veno-arterial ECMO (VA-ECMO) was performed at the bedside as a bridge-to-decision for advanced HF therapies. The IABP was left in place for LV venting. Within 72 hours, extensive bilateral pulmonary opacities had developed. It was later realized that true LV ejection (as evidenced by aortic pulsatility on the arterial line) was not present and had been masked by pseudo-pulsatility provided by IABP inflations and deflations. Compared to an echocardiogram done 7 days prior to VA-ECMO cannulation, the bioprosthetic leaflets were no longer opening, thrombosis of the AV had occurred, and thrombus formation along the ECMO venous drainage cannula was noted. Failure to achieve LV venting culminated in complete thrombosis of the entire LV and LA and the patient ultimately expired.
Discussion
Bioprosthetic valve thrombosis is a lesser-known complication of VA-ECMO support, with most reports involving bioprosthetic valves in the mitral position. Indeed, bioprosthetic valve thrombosis occurs at a higher rate than native valve thrombosis during VA-ECMO support. However, bioprosthetic AV thrombosis is an extremely rare complication of VA-ECMO support and arguably results in a more catastrophic scenario as most traditional approaches to LV unloading are contraindicated. The optimal LV unloading strategy for these patients (IABP, Impella, surgical apical unloading, etc) is unknown. Data from large retrospective analyses have demonstrated extremely poor outcomes when prosthetic valve thrombosis occurs, and it is thus critical to prevent this complication from developing. In contrast to IABP counter-pulsation, the benefit of upfront transvalvular LV venting with an Impella device safeguards the presence of a direct LV vent in the event of bioprosthetic AV thrombosis and eliminates the false reassurance of IABP pseudo-pulsatility. Further studies are needed to better elucidate the optimal LV unloading strategy in patients with bioprosthetic valves, particularly in the aortic position.
A 56-year-old male with a history of cardiac sarcoidosis with biventricular systolic heart failure (HF) and a bioprosthetic aortic valve presented with acute decompensated HF. Progressive cardiogenic shock and hemodynamic instability ensued, requiring urgent bedside placement of an intra-aortic balloon pump (IABP) which provided only marginal hemodynamic support. After extensive multidisciplinary discussion, emergent cannulation for veno-arterial ECMO (VA-ECMO) was performed at the bedside as a bridge-to-decision for advanced HF therapies. The IABP was left in place for LV venting. Within 72 hours, extensive bilateral pulmonary opacities had developed. It was later realized that true LV ejection (as evidenced by aortic pulsatility on the arterial line) was not present and had been masked by pseudo-pulsatility provided by IABP inflations and deflations. Compared to an echocardiogram done 7 days prior to VA-ECMO cannulation, the bioprosthetic leaflets were no longer opening, thrombosis of the AV had occurred, and thrombus formation along the ECMO venous drainage cannula was noted. Failure to achieve LV venting culminated in complete thrombosis of the entire LV and LA and the patient ultimately expired.
Discussion
Bioprosthetic valve thrombosis is a lesser-known complication of VA-ECMO support, with most reports involving bioprosthetic valves in the mitral position. Indeed, bioprosthetic valve thrombosis occurs at a higher rate than native valve thrombosis during VA-ECMO support. However, bioprosthetic AV thrombosis is an extremely rare complication of VA-ECMO support and arguably results in a more catastrophic scenario as most traditional approaches to LV unloading are contraindicated. The optimal LV unloading strategy for these patients (IABP, Impella, surgical apical unloading, etc) is unknown. Data from large retrospective analyses have demonstrated extremely poor outcomes when prosthetic valve thrombosis occurs, and it is thus critical to prevent this complication from developing. In contrast to IABP counter-pulsation, the benefit of upfront transvalvular LV venting with an Impella device safeguards the presence of a direct LV vent in the event of bioprosthetic AV thrombosis and eliminates the false reassurance of IABP pseudo-pulsatility. Further studies are needed to better elucidate the optimal LV unloading strategy in patients with bioprosthetic valves, particularly in the aortic position.
More abstracts on this topic:
Cerebral Oxygen Saturation for Early Prognostication Following Veno-Arterial Extracorporeal Membrane Oxygenation
Li Yi, Geng Cong, Chen Nan, Chen Hui, Huang Jian, Lu Shiqi, Zhang Ke
Assessing the Clinical Impact of Cardiac Intensivists in Cardiac Intensive Care Units.: Results from the RESCUE registryBae Dae-hwan, Bae Jang-whan, Lee Junyoung, Sun Jonghee, Lee Sang Yeub, Yang Jeong Hoon, Gwon Hyeon-cheol