Final ID: MDP375
Interoperable and Scalable Electronic Clinical Quality Measurement for Appropriate Use of Anticoagulation for Atrial Fibrillation in a Multicenter Health System
Abstract Body (Do not enter title and authors here): Background: Anticoagulation (AC) in patients with atrial fibrillation (AF) at high risk for stroke is strongly recommended in guidelines, but tracking the optimal use of AC at scale and across hospital systems is challenging due to the need to examine both thrombotic and bleeding risks that often factor in clinical decisions. We propose a novel electronic clinical quality measure (eCQM) based on a computable phenotyping algorithm developed for and applied to a common data model (CDM) to enable at-scale assessments of CHA2DS2VASc and HAS-BLED to patients with AF in a multi-hospital health system.
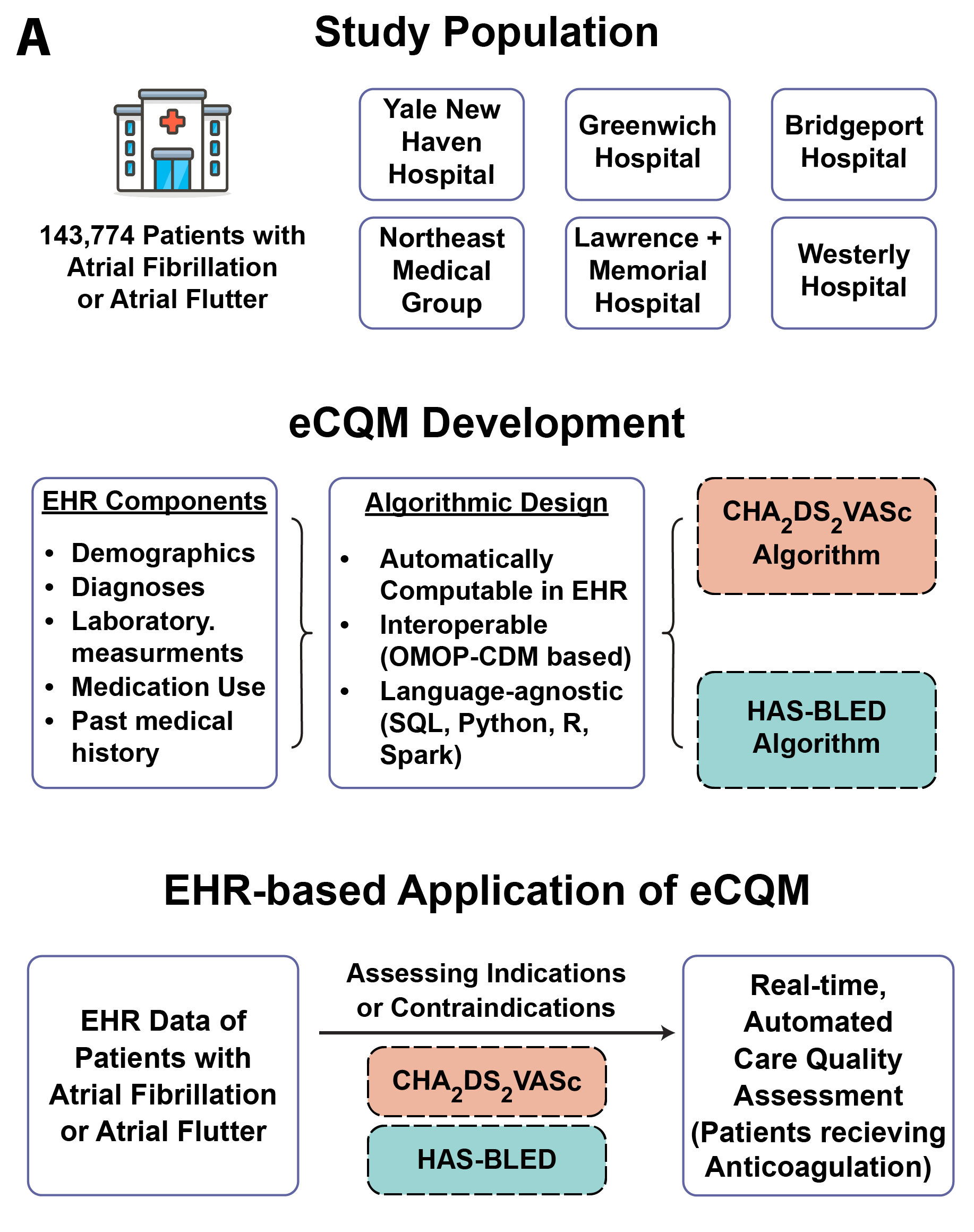
Methods: In patients with AF, we extracted CHA2DS2VASc and HAS-BLED scores by mapping individual components to standardized concepts from the Observational Medical Outcomes Partnership CDM concept set building tool, ATLAS. Clinician experts pursued manual curation of applicable concepts spanning demographics, conditions, laboratory values, medications, procedures, and vital signs, based on either the presence/absence of conditions in the patient EHR, or the given threshold of lab values or vital signs. We then assessed patients’ AC status across stroke and bleeding risk ranges [A].
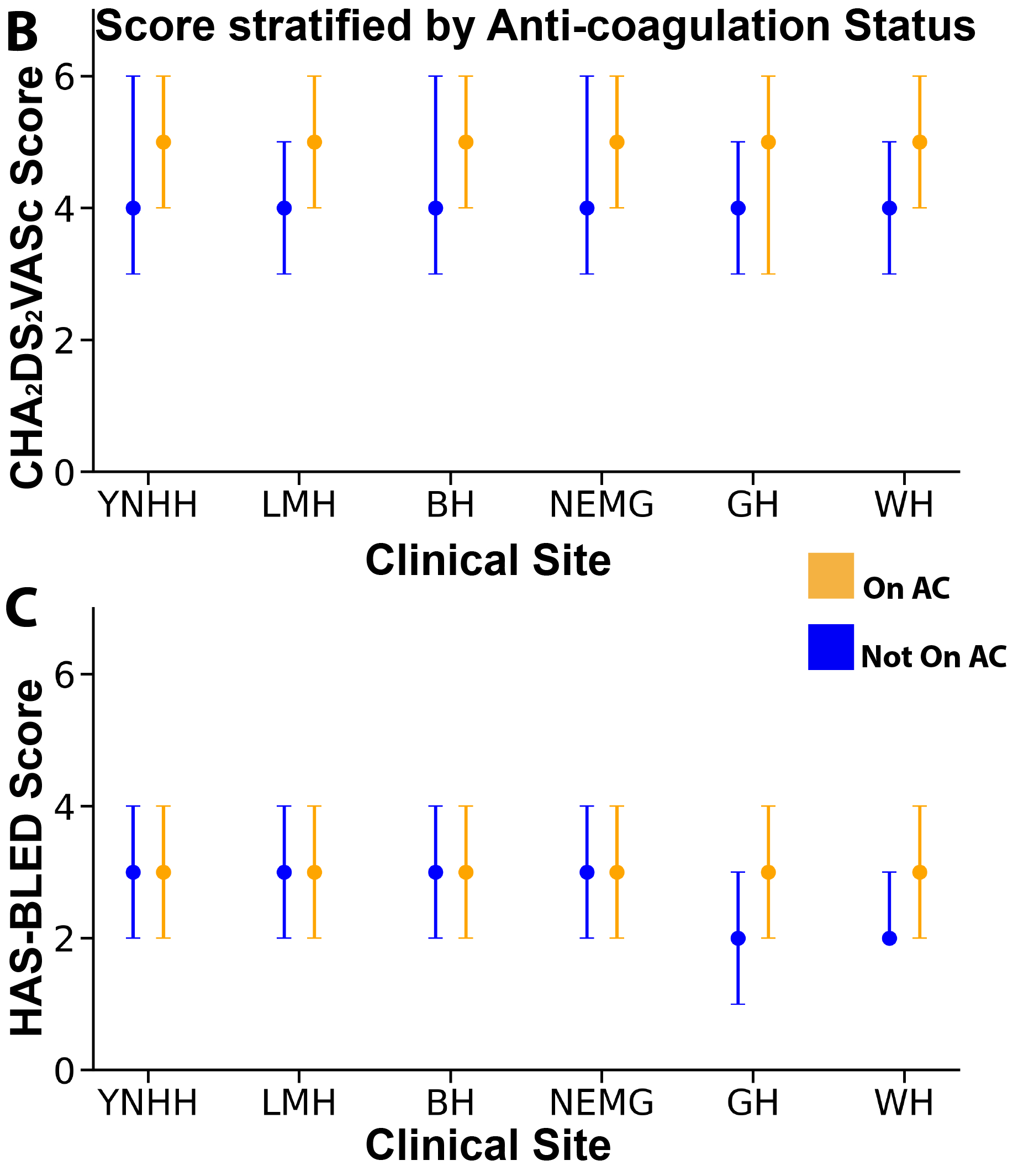
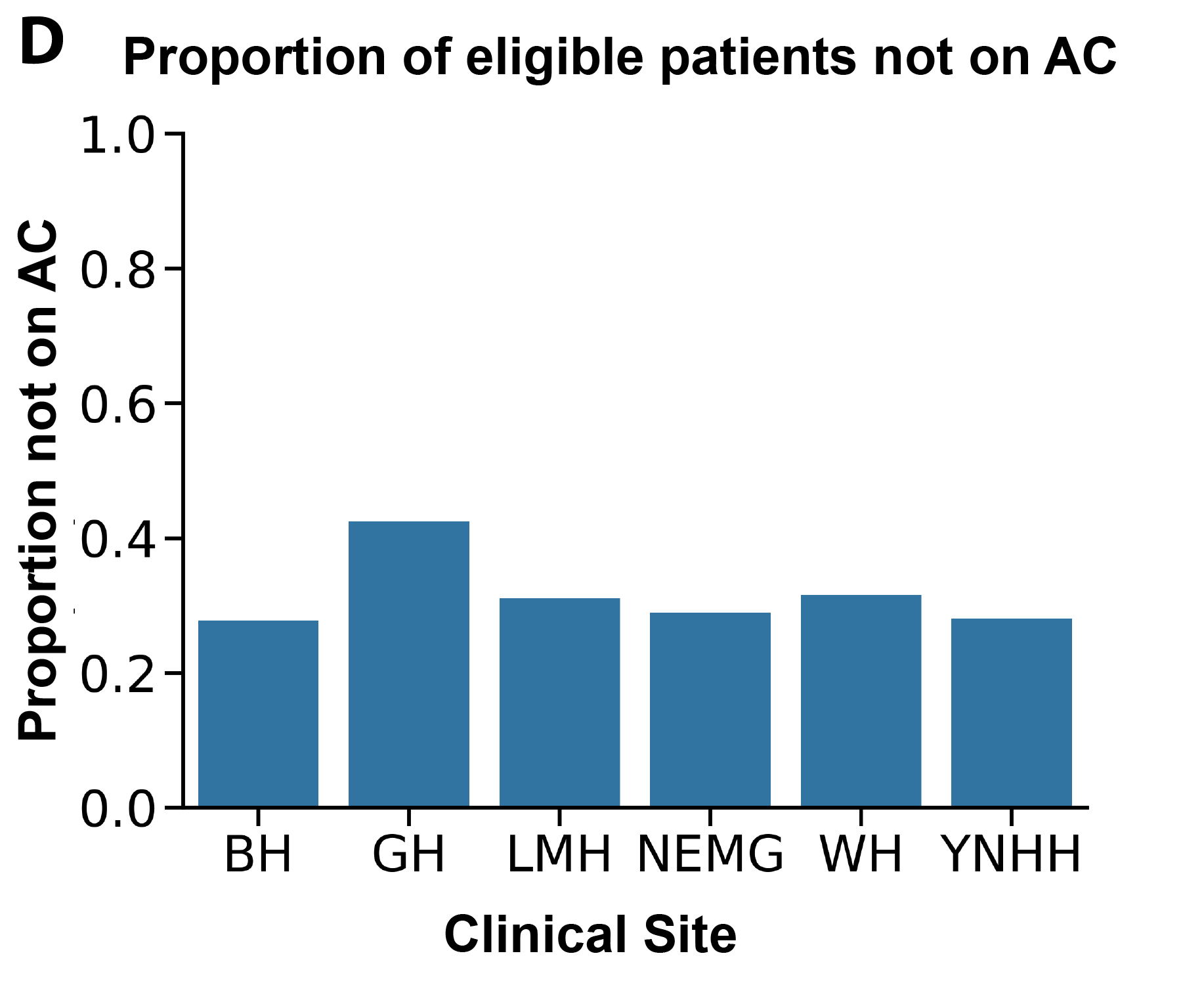
Results: Across 5 hospitals and clinic sites, there were 64,632 patients with AF, mean age 74 (SD 14) with 27,846 (43%) female, and 4,060 (8%) Black who interacted with the health system within the past year. The mean CHA2DS2VASc score was 4.5 (SD 2.0) and HAS-BLED was 3.0 (SD 1.5). For those on AC, the mean CHA2DS2VASc score was 4.8 (SD 2.0) versus 3.8 (SD 2.1) for those not on AC [B], while the mean HAS-BLED score for those on AC was 3.2 (SD 1.5) vs 2.7 (SD 1.5) for those not on AC [C]. By score, 92% had a stroke risk of 2% or greater, and 66% of these patients were on AC, with a mean HAS-BLED score of 3.2 (SD 1.5). The most common contributors to a HAS-BLED score of 2 or greater were medication exposure predisposing to bleeding (90%), age greater than 65 (85%), prior bleeding event (47%), and uncontrolled hypertension (46%). Across hospital sites, the proportion of patients with AF with a CHA2DS2VASc score of 2 or more and HAS-BLED score of 4 or less not on AC varied from 58% (Greenwich Hospital) to 72% (Bridgeport Hospital) [D].
Conclusion: We demonstrate the ability of a scalable EHR-native eCQM that accounts for thrombotic and bleeding risk at scale to monitor the quality of care, with gaps in care noted in a large diverse health system.
Methods: In patients with AF, we extracted CHA2DS2VASc and HAS-BLED scores by mapping individual components to standardized concepts from the Observational Medical Outcomes Partnership CDM concept set building tool, ATLAS. Clinician experts pursued manual curation of applicable concepts spanning demographics, conditions, laboratory values, medications, procedures, and vital signs, based on either the presence/absence of conditions in the patient EHR, or the given threshold of lab values or vital signs. We then assessed patients’ AC status across stroke and bleeding risk ranges [A].
Results: Across 5 hospitals and clinic sites, there were 64,632 patients with AF, mean age 74 (SD 14) with 27,846 (43%) female, and 4,060 (8%) Black who interacted with the health system within the past year. The mean CHA2DS2VASc score was 4.5 (SD 2.0) and HAS-BLED was 3.0 (SD 1.5). For those on AC, the mean CHA2DS2VASc score was 4.8 (SD 2.0) versus 3.8 (SD 2.1) for those not on AC [B], while the mean HAS-BLED score for those on AC was 3.2 (SD 1.5) vs 2.7 (SD 1.5) for those not on AC [C]. By score, 92% had a stroke risk of 2% or greater, and 66% of these patients were on AC, with a mean HAS-BLED score of 3.2 (SD 1.5). The most common contributors to a HAS-BLED score of 2 or greater were medication exposure predisposing to bleeding (90%), age greater than 65 (85%), prior bleeding event (47%), and uncontrolled hypertension (46%). Across hospital sites, the proportion of patients with AF with a CHA2DS2VASc score of 2 or more and HAS-BLED score of 4 or less not on AC varied from 58% (Greenwich Hospital) to 72% (Bridgeport Hospital) [D].
Conclusion: We demonstrate the ability of a scalable EHR-native eCQM that accounts for thrombotic and bleeding risk at scale to monitor the quality of care, with gaps in care noted in a large diverse health system.
More abstracts on this topic:
Impact of Myocardial Injury Assessment in Emergency Department on Disposition Distribution and Time to Disposition
Landry Alexander, Defilippis Andrew, Michael Kirolos, Lidani Karita, Palmer Benjamin, Tomar Shubham, Xu Meng, Libre Michael, Sexton Mitchell, Wrenn Jesse
Association of Non-Cardiac Comorbidities With Long-Term Re-Hospitalization for Heart Failure: Contemporary Analysis of 88,528 Consecutive CasesAmbrosio Giuseppe, Tagliabue Elena, Pellicori Pierpaolo, Lund Lars, Pontiroli Antonio