Final ID: Sa3168
A quality improvement intervention and academic detailing vs. academic detailing alone, a randomized quality improvement study
Abstract Body (Do not enter title and authors here): Background: Appropriate direct oral anticoagulants (DOAC) dosing could improve their safety and effectiveness. To address this, we developed an intervention to improve on-label dosing using academic detailing and a quality improvement intervention.
Methods: This was a cluster RCT with clusters at the site level. There were 2 arms, academic detailing (AD) and AD plus Learn. Engage. Act. Process. (AD/LEAP).
Interventions: Primary care doctors and anticoagulation pharmacists from all participating sites were invited to participate in academic detailing, a 1:1 educational and motivational coaching program, about ways to improve DOAC prescribing safely.
Intervention arm sites were also invited to participate in LEAP, a quality improvement program based on plan-do-study-act cycles.
Sites: 8 VA medical centers
Inclusion criteria: All patients on DOACs at participating sites.
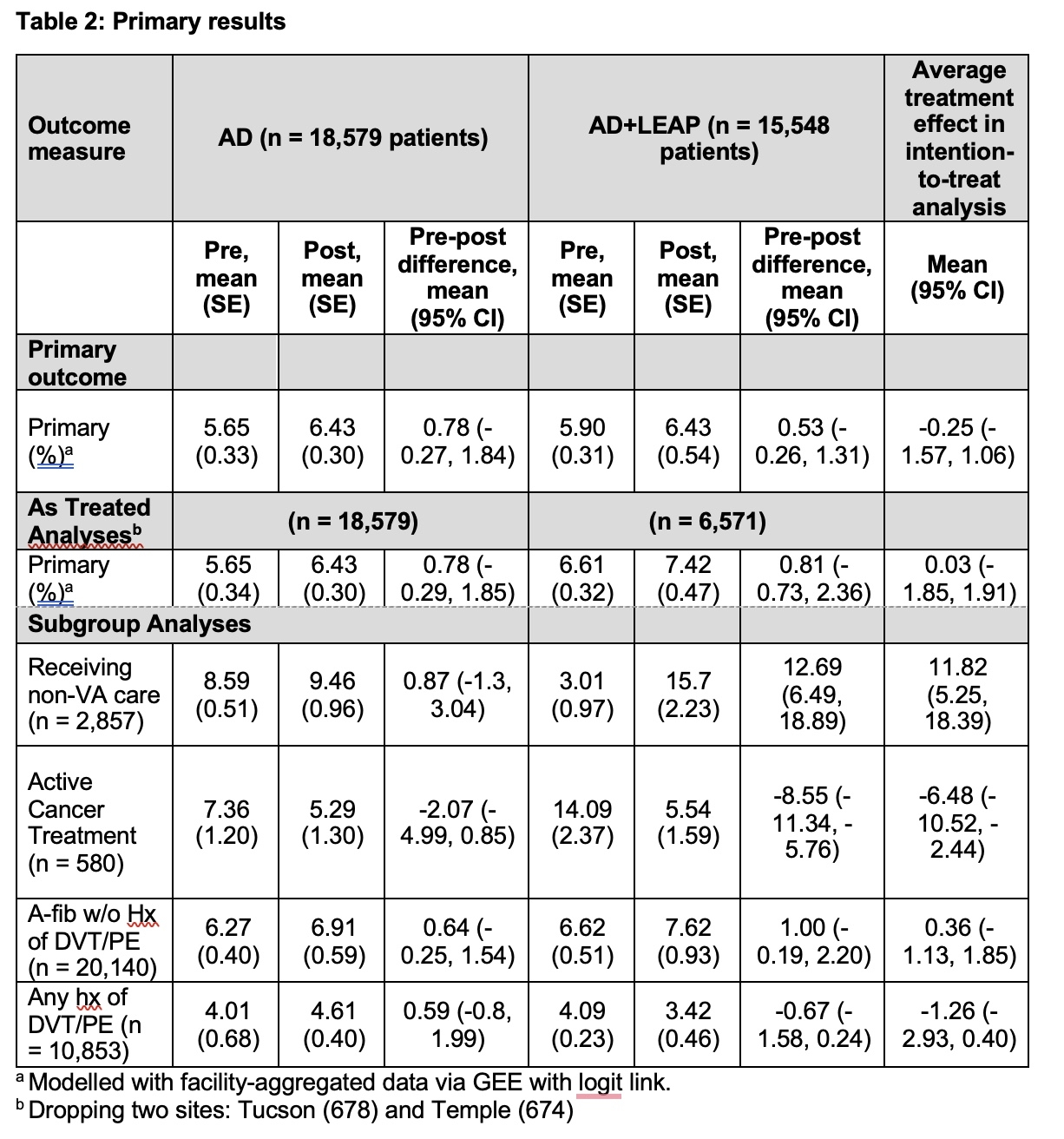
Analysis: Generalized Estimating Equations with logit links and clusters at the facility level using aggregated proportion data. Models were weighted by the size of the denominator within each facility and longitudinal measurements were modeled with an autoregressive working correlation matrix. For difference-in-difference modeling, the 6-month pre- and post-period data were included and entered into the model as a fixed effect plus an interaction with the treatment arm.
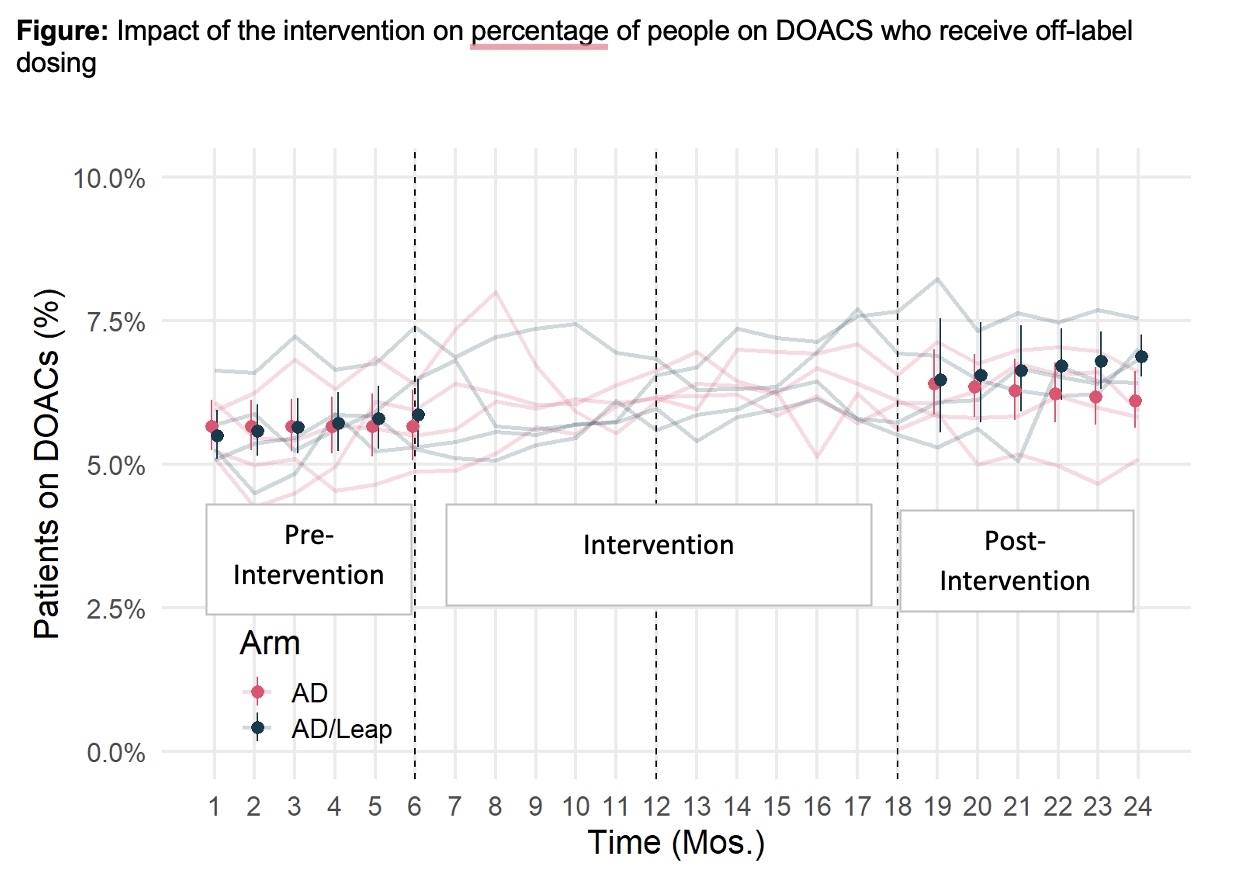
Outcomes: The primary outcome was the percentage of DOAC prescribing that was off-label, including under- and over-dosing for that individual and using for inappropriate indications.
Results: Over the full length of the study, there were 34,127 patients on DOACs across the 8 sites. The percentage of prescriptions that met the primary outcome increased from 5.65 to 6.43 in the AD arm and from 5.9 to 6.43 in the AD+LEAP arm, yielding a difference-in-difference of -0.25 (95% CI -1.57- 1.06). An as-treated analysis, which dropped the two sites that did not finish their LEAP programs, also found no effect, as did sub-groups of impacts on patients whose reason for using DOACs was atrial fibrillation vs. thromboembolism.
Discussion: A quality improvement intervention did not improve safe DOAC prescribing when added to an academic detailing intervention. We hypothesize the primary reason was insufficient engagement with the intervention.
Methods: This was a cluster RCT with clusters at the site level. There were 2 arms, academic detailing (AD) and AD plus Learn. Engage. Act. Process. (AD/LEAP).
Interventions: Primary care doctors and anticoagulation pharmacists from all participating sites were invited to participate in academic detailing, a 1:1 educational and motivational coaching program, about ways to improve DOAC prescribing safely.
Intervention arm sites were also invited to participate in LEAP, a quality improvement program based on plan-do-study-act cycles.
Sites: 8 VA medical centers
Inclusion criteria: All patients on DOACs at participating sites.
Analysis: Generalized Estimating Equations with logit links and clusters at the facility level using aggregated proportion data. Models were weighted by the size of the denominator within each facility and longitudinal measurements were modeled with an autoregressive working correlation matrix. For difference-in-difference modeling, the 6-month pre- and post-period data were included and entered into the model as a fixed effect plus an interaction with the treatment arm.
Outcomes: The primary outcome was the percentage of DOAC prescribing that was off-label, including under- and over-dosing for that individual and using for inappropriate indications.
Results: Over the full length of the study, there were 34,127 patients on DOACs across the 8 sites. The percentage of prescriptions that met the primary outcome increased from 5.65 to 6.43 in the AD arm and from 5.9 to 6.43 in the AD+LEAP arm, yielding a difference-in-difference of -0.25 (95% CI -1.57- 1.06). An as-treated analysis, which dropped the two sites that did not finish their LEAP programs, also found no effect, as did sub-groups of impacts on patients whose reason for using DOACs was atrial fibrillation vs. thromboembolism.
Discussion: A quality improvement intervention did not improve safe DOAC prescribing when added to an academic detailing intervention. We hypothesize the primary reason was insufficient engagement with the intervention.
More abstracts on this topic:
Among Older Adults With Atrial Fibrillation, First Anticoagulant Prescription Is Not Associated with Reduced Hazard of Ischemic Stroke but Is Associated with Increased Hazard of Major Bleeding: A Nationwide Study
Lusk Jay, Li Fan, Mac Grory Brian, Nalawade Vinit, Wilson Lauren, Yarnell Stephanie, Song Ailin, Schrag Matthew, Poli Sven, Hammill Bradley, Xian Ying
A Meta-Analysis of Randomized Controlled Trials: Aldosterone Synthase Inhibitors as a Therapeutic Strategy for HypertensionMarzano Luigi, Merlo Matteo, Pizzolo Francesca, Friso Simonetta