Final ID: Su3101
Maternal Nativity and Adverse Pregnancy Outcomes Stratified by Maternal Race/Ethnicity: Insights from the National Vital Statistics System
Abstract Body (Do not enter title and authors here): Background
Adverse pregnancy outcomes (APOs) are a major cause of maternal morbidity and mortality, with significant variations in APOs prevalence among racial and ethnic groups. The US has rising immigration rates. Currently, studies with national representation are limited to detect the association of nativity with APOs.
Objective
To determine the association between maternal nativity and APOs across maternal race and ethnicity groups in the US.
Methods
We conducted a nationwide, cross-sectional study using data from the National Vital Statistics System natality files, encompassing all live births in the US from 2016 to 2022 among individuals aged 15 - 44 years. Maternal nativity was classified as non–US-born vs US-born. The outcomes of interest (APOs) included gestational diabetes mellitus (GDM), hypertensive disorders of pregnancy (HDP), and pre-term birth (PTB). Multivariable logistic regression was used to determine the association between maternal nativity and APOs, stratified by race and ethnicity, including Asian, Black, Hispanic, White, or other (individuals who selected other race or more than one race).
Results
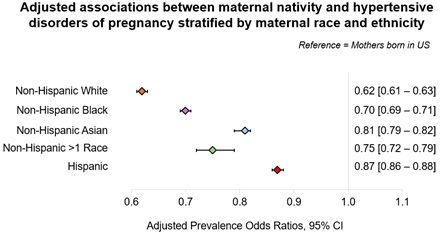
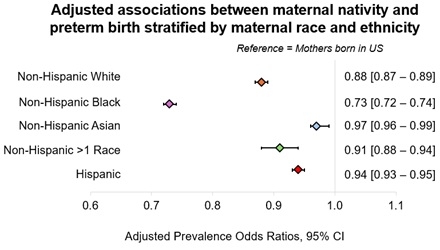
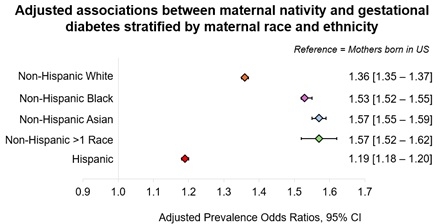
24,366,281 birthing individuals were included. Non-US-born individuals had lower prevalence odds ratio of HDP (adjusted prevalence odds ratio (aPOR) 0.689 [95% CI 0.686-0.692]) and PTB (aPOR 0.922 [95% CI 0.919-0.925]) compared to US-born individuals, which was consistent across the majority of race and ethnicity groups (Figure 1, 2 &3). However, non-US-born individuals experienced significantly higher POR for GDM (aPOR 1.70 [95% CI 1.69-1.70]) (Figure 1, 2 &3).
Conclusions
Individuals born outside the US have higher odds of GDM, but lower odds for HDP and PTB. Findings suggest that APO risk may be environmentally influenced beyond genetic ancestry, with different risk factors geographically across the world.
Adverse pregnancy outcomes (APOs) are a major cause of maternal morbidity and mortality, with significant variations in APOs prevalence among racial and ethnic groups. The US has rising immigration rates. Currently, studies with national representation are limited to detect the association of nativity with APOs.
Objective
To determine the association between maternal nativity and APOs across maternal race and ethnicity groups in the US.
Methods
We conducted a nationwide, cross-sectional study using data from the National Vital Statistics System natality files, encompassing all live births in the US from 2016 to 2022 among individuals aged 15 - 44 years. Maternal nativity was classified as non–US-born vs US-born. The outcomes of interest (APOs) included gestational diabetes mellitus (GDM), hypertensive disorders of pregnancy (HDP), and pre-term birth (PTB). Multivariable logistic regression was used to determine the association between maternal nativity and APOs, stratified by race and ethnicity, including Asian, Black, Hispanic, White, or other (individuals who selected other race or more than one race).
Results
24,366,281 birthing individuals were included. Non-US-born individuals had lower prevalence odds ratio of HDP (adjusted prevalence odds ratio (aPOR) 0.689 [95% CI 0.686-0.692]) and PTB (aPOR 0.922 [95% CI 0.919-0.925]) compared to US-born individuals, which was consistent across the majority of race and ethnicity groups (Figure 1, 2 &3). However, non-US-born individuals experienced significantly higher POR for GDM (aPOR 1.70 [95% CI 1.69-1.70]) (Figure 1, 2 &3).
Conclusions
Individuals born outside the US have higher odds of GDM, but lower odds for HDP and PTB. Findings suggest that APO risk may be environmentally influenced beyond genetic ancestry, with different risk factors geographically across the world.
More abstracts on this topic:
Depressive symptoms during late pregnancy are associated with higher cardiovascular disease risk 2-7 years after delivery.
Donofry Shannon, Yee Lynn, Catov Janet, Grobman William, Bairey Merz C Noel, Saade George, Hoffman Matthew, Pemberton Victoria, Levine Lisa, Khan Sadiya, Reddy Uma
Gestational Diabetes and Risk of Type 2 Diabetes: Exploring the Role of Gut microbiome and Blood Metabolome in the Hispanic Community Health Study / Study of Latinos (HCHS/SOL)Wang Yi, Peters-samuelson Brandilyn, Isasi Carmen, Stuebe Alison, Louis-jacques Adetola, Daviglus Martha, Boerwinkle Eric, Burk Robert, Kaplan Robert, Qi Qibin