Final ID: Mo4144
Impact of Left Ventricular Diastolic Function in Pulmonary Arterial Hypertension Outcomes
Abstract Body (Do not enter title and authors here): Introduction: The demographics of patients with pulmonary arterial hypertension (PAH) is shifting towards older age, increased comorbidity burden, and an increase in the risk of left ventricular (LV) diastolic dysfunction. The H2FPEF score and probability were developed to assist in heart failure with preserved ejection fraction (HFpEF) diagnosis. We evaluated the utility of the H2FPEF score as well as echocardiographic measures of LV diastolic function in PAH.
Hypothesis: Development of left-sided heart failure in a population of patients diagnosed with PAH may affect outcomes for those treated with PAH based therapies.
Methods: Participants with an inpatient admission and a prostacyclin order at the Ohio State University Medical Center between Jan 2020 and Dec. 2022 were included. Chart review was performed to obtain clinical and echocardiographic data. The H2FPEF score and probability were calculated at the time of the Echo. Survival analysis was performed (Outcome: PAH related-hospitalization or death). Significant predictors of outcomes were identified using Cox logistic regression analysis. Data are presented as mean ± standard deviation or mean [interquartile range].
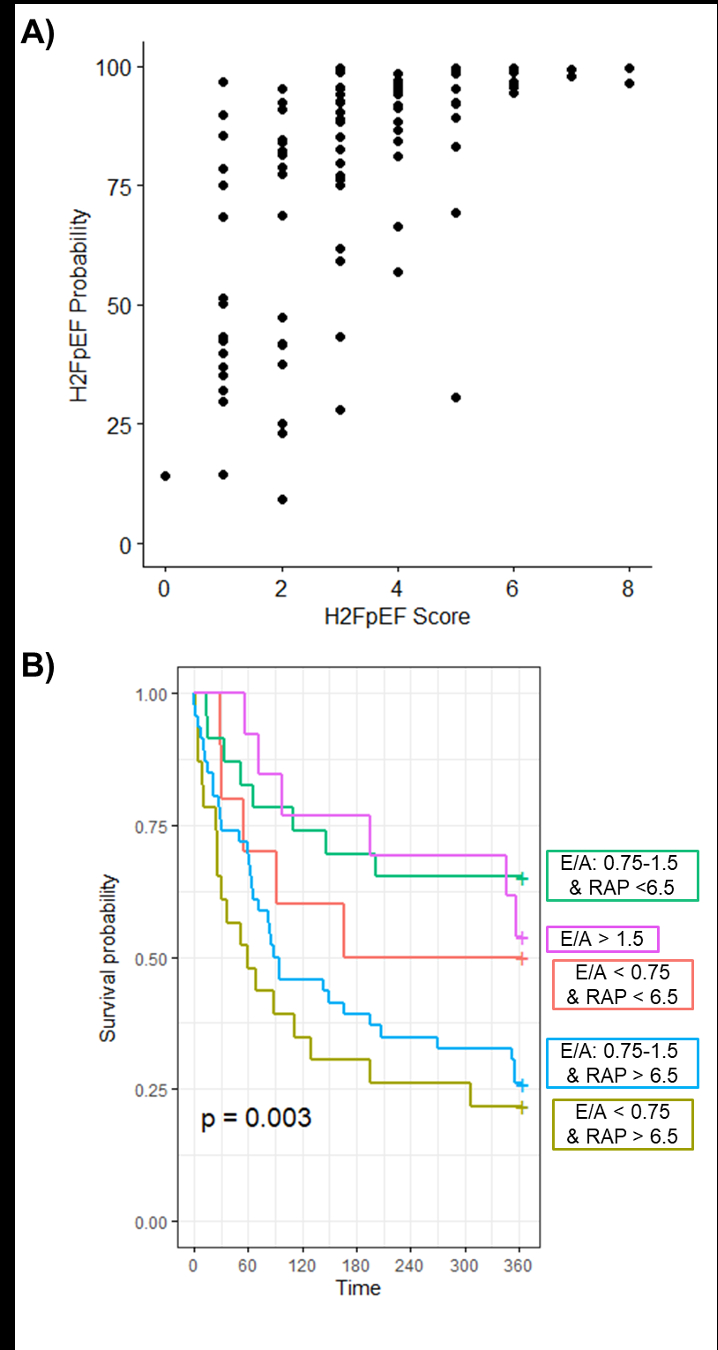
Results: Overall, 140 participants were identified (age: 56±16 years; BMI: 30.04±8.04 kg/m2; 74% female) with normal left ejection fraction (LVEF: 63±9%). The majority were on prostacyclin therapy or no therapy at the time of the echo. Median H2FPEF score was 3[2-4] and median H2FPEF probability was 88[67-95%]. High H2FPEF probability was driven by high systolic PA pressure (70±22 mmHg) in the continuous equation (Fig 1A). The H2FPEF score and probability did not associate with outcomes. However, E/A ratio (HR:0.49(0.26-0.92), p=0.03) and estimated RA pressure (HR:1.1(1-1.1), p=0.02) did significantly associate with outcomes individually and in a multivariable assessment with adjusting for age and BMI (Fig 1B).
Conclusions: The continuous H2FPEF probability did not perform well in this inpatient PAH cohort primarily on prostacyclin therapy. Notably measures of right and left atrial function (E/A and estimated RA pressure) did significantly associate with hospitalization and mortality. Future studies in a broader cohort of PAH patients are needed to better understand how diastolic function parameters may impact outcomes.
Hypothesis: Development of left-sided heart failure in a population of patients diagnosed with PAH may affect outcomes for those treated with PAH based therapies.
Methods: Participants with an inpatient admission and a prostacyclin order at the Ohio State University Medical Center between Jan 2020 and Dec. 2022 were included. Chart review was performed to obtain clinical and echocardiographic data. The H2FPEF score and probability were calculated at the time of the Echo. Survival analysis was performed (Outcome: PAH related-hospitalization or death). Significant predictors of outcomes were identified using Cox logistic regression analysis. Data are presented as mean ± standard deviation or mean [interquartile range].
Results: Overall, 140 participants were identified (age: 56±16 years; BMI: 30.04±8.04 kg/m2; 74% female) with normal left ejection fraction (LVEF: 63±9%). The majority were on prostacyclin therapy or no therapy at the time of the echo. Median H2FPEF score was 3[2-4] and median H2FPEF probability was 88[67-95%]. High H2FPEF probability was driven by high systolic PA pressure (70±22 mmHg) in the continuous equation (Fig 1A). The H2FPEF score and probability did not associate with outcomes. However, E/A ratio (HR:0.49(0.26-0.92), p=0.03) and estimated RA pressure (HR:1.1(1-1.1), p=0.02) did significantly associate with outcomes individually and in a multivariable assessment with adjusting for age and BMI (Fig 1B).
Conclusions: The continuous H2FPEF probability did not perform well in this inpatient PAH cohort primarily on prostacyclin therapy. Notably measures of right and left atrial function (E/A and estimated RA pressure) did significantly associate with hospitalization and mortality. Future studies in a broader cohort of PAH patients are needed to better understand how diastolic function parameters may impact outcomes.
More abstracts on this topic:
Acute Administration of The Novel Cardiac Sarcomere Modulator EDG-7500, Improves Ventricular Filling While Preserving LVEF In Dogs with Pacing Induced Left-Ventricular Systolic Dysfunction
Evanchik Marc, Emter Craig, Del Rio Carlos, Roof Steve, St Clair Sydney, Russell Alan, Henze Marcus, Semigran Marc
A Novel EMR-Based Algorithm with the Virtual Echocardiography Screening Tool (VEST) to Screen Patients for Pulmonary Arterial HypertensionNarowska Gabriela, Anand Suneesh, Gangireddy Chethan, Enevoldsen John, Keane Martin, Edmundowicz Daniel, Forfia Paul, Vaidya Anjali