Final ID: Su4108
Outcomes of Transcatheter Aortic Valve Implantation (TAVI) in Patients with and without Iron Deficiency Anemia: An Analysis of the National Inpatient Sample (NIS) Data from 2016-2021
Abstract Body (Do not enter title and authors here): Background:
Iron deficiency anemia (IDA) is a common comorbidity in patients undergoing Transcatheter Aortic Valve Implantation (TAVI). This study investigates the differences in outcomes between TAVI patients with and without IDA, focusing on mortality, procedural complications, and baseline characteristics.
Methods:
A retrospective analysis was conducted using data from the National Inpatient Sample (NIS) from 2016 to 2021. The outcomes for patients undergoing TAVI with IDA were compared to those without IDA. Multivariate logistic regression was employed to analyze outcomes.
Results:
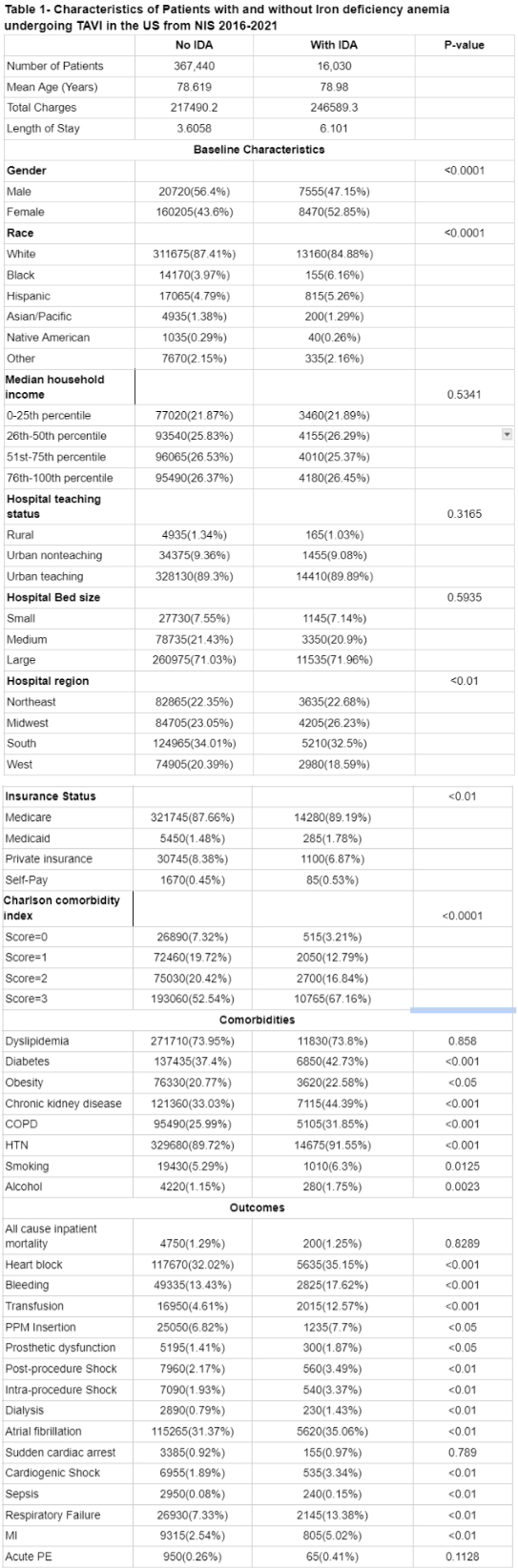
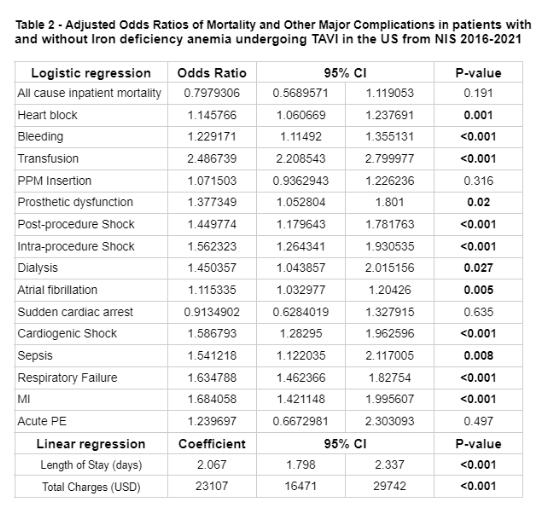
The study included 367,440 patients without iron deficiency anemia and 16,030 patients with iron deficiency anemia. Baseline characteristics showed a significant difference in gender distribution, with 47.15% of IDA patients being male compared to 56.4% in the non-IDA group (P < 0.0001). Racial distribution varied significantly (P < 0.0001), with a higher % of Black patients in the IDA group (6.16% vs. 3.97%).Patients with IDA had higher odds of heart block (OR: 1.146, 95% CI: 1.061-1.238, P = 0.001), bleeding (OR: 1.229, 95% CI: 1.115-1.355, P < 0.001), transfusion (OR: 2.487, 95% CI: 2.209-2.800, P < 0.001), prosthetic dysfunction (OR: 1.377, 95% CI: 1.053-1.801, P = 0.02), post-procedure shock (OR: 1.450, 95% CI: 1.180-1.782, P < 0.001), intra-procedure shock (OR: 1.562, 95% CI: 1.264-1.931, P < 0.001), dialysis (OR: 1.450, 95% CI: 1.044-2.015, P = 0.027), atrial fibrillation (OR: 1.115, 95% CI: 1.033-1.204, P = 0.005), cardiogenic shock (OR: 1.587, 95% CI: 1.283-1.963, P < 0.001), sepsis (OR: 1.541, 95% CI: 1.122-2.117, P = 0.008), respiratory failure (OR: 1.635, 95% CI: 1.462-1.828, P < 0.001), and myocardial infarction (OR: 1.684, 95% CI: 1.421-1.996, P < 0.001). .Patients with IDA had a longer length of stay (Coefficient: 2.067, 95% CI: 1.798-2.337, P < 0.001) and higher total hospital charges (Coefficient: $23,107, 95% CI: $16,471-$29,742, P < 0.001) compared to those without IDA.
Conclusions:
Patients with IDA undergoing TAVI are at higher risk for several complications, including heart block, bleeding, transfusion, prosthetic dysfunction, post-procedure and intra-procedure shock, dialysis, atrial fibrillation, cardiogenic shock, sepsis, respiratory failure, and myocardial infarction compared to those without IDA. These findings underscore the need for targeted management strategies and further research to optimize outcomes for TAVI patients with iron deficiency anemia.
Iron deficiency anemia (IDA) is a common comorbidity in patients undergoing Transcatheter Aortic Valve Implantation (TAVI). This study investigates the differences in outcomes between TAVI patients with and without IDA, focusing on mortality, procedural complications, and baseline characteristics.
Methods:
A retrospective analysis was conducted using data from the National Inpatient Sample (NIS) from 2016 to 2021. The outcomes for patients undergoing TAVI with IDA were compared to those without IDA. Multivariate logistic regression was employed to analyze outcomes.
Results:
The study included 367,440 patients without iron deficiency anemia and 16,030 patients with iron deficiency anemia. Baseline characteristics showed a significant difference in gender distribution, with 47.15% of IDA patients being male compared to 56.4% in the non-IDA group (P < 0.0001). Racial distribution varied significantly (P < 0.0001), with a higher % of Black patients in the IDA group (6.16% vs. 3.97%).Patients with IDA had higher odds of heart block (OR: 1.146, 95% CI: 1.061-1.238, P = 0.001), bleeding (OR: 1.229, 95% CI: 1.115-1.355, P < 0.001), transfusion (OR: 2.487, 95% CI: 2.209-2.800, P < 0.001), prosthetic dysfunction (OR: 1.377, 95% CI: 1.053-1.801, P = 0.02), post-procedure shock (OR: 1.450, 95% CI: 1.180-1.782, P < 0.001), intra-procedure shock (OR: 1.562, 95% CI: 1.264-1.931, P < 0.001), dialysis (OR: 1.450, 95% CI: 1.044-2.015, P = 0.027), atrial fibrillation (OR: 1.115, 95% CI: 1.033-1.204, P = 0.005), cardiogenic shock (OR: 1.587, 95% CI: 1.283-1.963, P < 0.001), sepsis (OR: 1.541, 95% CI: 1.122-2.117, P = 0.008), respiratory failure (OR: 1.635, 95% CI: 1.462-1.828, P < 0.001), and myocardial infarction (OR: 1.684, 95% CI: 1.421-1.996, P < 0.001). .Patients with IDA had a longer length of stay (Coefficient: 2.067, 95% CI: 1.798-2.337, P < 0.001) and higher total hospital charges (Coefficient: $23,107, 95% CI: $16,471-$29,742, P < 0.001) compared to those without IDA.
Conclusions:
Patients with IDA undergoing TAVI are at higher risk for several complications, including heart block, bleeding, transfusion, prosthetic dysfunction, post-procedure and intra-procedure shock, dialysis, atrial fibrillation, cardiogenic shock, sepsis, respiratory failure, and myocardial infarction compared to those without IDA. These findings underscore the need for targeted management strategies and further research to optimize outcomes for TAVI patients with iron deficiency anemia.
More abstracts on this topic:
Association Between Pre-Existing Chronic Total Occlusion and Post-TAVR Pacemaker Implantation: A Retrospective Propensity Matched Analysis
Haseeb Shahan, Ansari Umair, Munir Shafia, Lee Sang, Chan Marvyn, Goldbarg Seth
Aortic Root Pressure for Detecting Aortic Stenosis using Machine LearningDunn Michael, Lalush David, Wheaten Sterling, Stouffer George, Syed Faisal