Final ID: Mo4102
Evaluating Complications And Healthcare Utilization Of Intravascular Ultrasound Guided Percutaneous Coronary Interventions: A Retrospective Observational Study
Abstract Body (Do not enter title and authors here):
Background:
While using intravenous ultrasound(IVUS) during Percutaneous interventions(PCI) enhances lesion assessment, stent placement, and procedural precision, it may also potentially increase procedural costs and complications.
Research Question:
This study aims to evaluate the outcomes, complications, and healthcare utilization associated with IVUS-guided PCI.
Method:
We conducted our study utilizing data from the nationwide inpatient sample database from January 2016 to December 2020. The study cohort comprised 444,571 hospitalized patients who underwent PCI during their hospitalization. We compared the outcomes of interventions with the use of IVUS and those without. The primary outcome was inpatient mortality. Secondary outcomes were the length of stay, cost of hospitalization, in-hospital and procedural complications as well as the need for life-saving interventions.
Results:
Among 444,571 patients who underwent PCI, 37,482(8.4%) had IVUS used during their procedure. Among the study population, 67.3% were male, 75.4% were white, 9.5% were black and the remaining 15.1% comprised of other races. The average age of the population was 65.37 years. All outcomes in this study were adjusted for age, race, sex, and comorbidities using the Charlson comorbidity index.
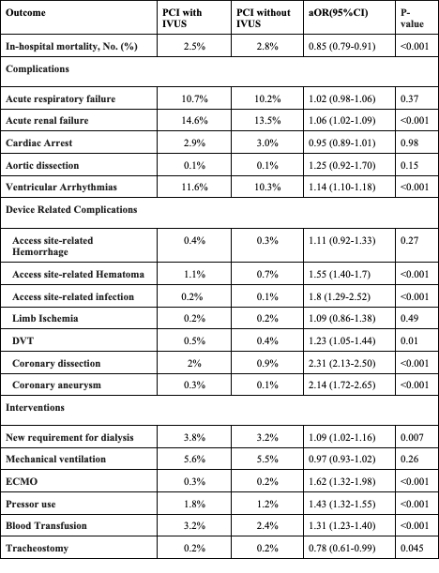
Cases that utilized IVUS experienced a significant reduction in in-patient mortality. However, they did have an increased risk of acute renal failure and ventricular arrhythmias. There was also an increase in procedure-related complications like access site-related hematoma, access site-related infection, deep venous thrombosis, coronary artery dissection, and coronary artery aneurysm. They also had an increased need for interventions like dialysis, extra-corporeal membrane oxygenation, pressors, and blood transfusions. Additionally, this group also had a significantly higher length of stay (mean 5.2 days vs. 4.9 days, p<0.001), and cost of hospitalization ($134,914 vs. $117,411, p<0.001).
Conclusion:
Although IVUS-guided PCI is linked to an uptick in certain complications and overall healthcare costs, it concurrently shows a decrease in in-hospital mortality. This contrast paints a complex picture; the modest increase in risk is counterbalanced by a critical mortality benefit. Ultimately, the benefits of potentially improved survival rates may justify the use of IVUS in PCI, particularly in settings where precision and detailed assessment can significantly impact patient outcomes.
Background:
While using intravenous ultrasound(IVUS) during Percutaneous interventions(PCI) enhances lesion assessment, stent placement, and procedural precision, it may also potentially increase procedural costs and complications.
Research Question:
This study aims to evaluate the outcomes, complications, and healthcare utilization associated with IVUS-guided PCI.
Method:
We conducted our study utilizing data from the nationwide inpatient sample database from January 2016 to December 2020. The study cohort comprised 444,571 hospitalized patients who underwent PCI during their hospitalization. We compared the outcomes of interventions with the use of IVUS and those without. The primary outcome was inpatient mortality. Secondary outcomes were the length of stay, cost of hospitalization, in-hospital and procedural complications as well as the need for life-saving interventions.
Results:
Among 444,571 patients who underwent PCI, 37,482(8.4%) had IVUS used during their procedure. Among the study population, 67.3% were male, 75.4% were white, 9.5% were black and the remaining 15.1% comprised of other races. The average age of the population was 65.37 years. All outcomes in this study were adjusted for age, race, sex, and comorbidities using the Charlson comorbidity index.
Cases that utilized IVUS experienced a significant reduction in in-patient mortality. However, they did have an increased risk of acute renal failure and ventricular arrhythmias. There was also an increase in procedure-related complications like access site-related hematoma, access site-related infection, deep venous thrombosis, coronary artery dissection, and coronary artery aneurysm. They also had an increased need for interventions like dialysis, extra-corporeal membrane oxygenation, pressors, and blood transfusions. Additionally, this group also had a significantly higher length of stay (mean 5.2 days vs. 4.9 days, p<0.001), and cost of hospitalization ($134,914 vs. $117,411, p<0.001).
Conclusion:
Although IVUS-guided PCI is linked to an uptick in certain complications and overall healthcare costs, it concurrently shows a decrease in in-hospital mortality. This contrast paints a complex picture; the modest increase in risk is counterbalanced by a critical mortality benefit. Ultimately, the benefits of potentially improved survival rates may justify the use of IVUS in PCI, particularly in settings where precision and detailed assessment can significantly impact patient outcomes.
More abstracts on this topic:
MDA-LDL levels and Histological Investigation of IVUS and Thrombus Aspiration Tissue in Patients undergoing Emergency Percutaneous Coronary Angioplasty for ACS
Suzuki Hiroko, Terajima Yutaka, Sato Kayoko, Miyoshino Hazime, Ono Manami, Fujita Motohiro, Fukushima Hiroshi, Kikuchi Yasuhiro, Kimura Yuya, Arai Kiyohito
A Non-odorant Olfactory Receptor Ligand Depolymerizes the Platelet Actin Cytoskeleton to Prevent ThrombosisAggarwal Anu, Godwin Matthew, Ali Mariya, Jennings Courtney, Rajasekar Bhairavi, Scalise Alliefair, Stauffer Shaun, Mccrae Keith, Mcintyre Thomas, Cameron Scott, Wang Nancy, Josyula Vara Prasad, Yang Moua, Young Shim, Kennedy Quinn, Samuel Reina, Sangwan Naseer, Guntupalli Suman