Final ID: Su2129
Exploring Optimal Cardiac Electronic Implantable Devices Programming: Reducing Non-Actionable Alerts and Assessing Clinical Outcomes
Abstract Body (Do not enter title and authors here): Background: Remote monitoring for cardiac electronic implantable devices (CIEDs) has become standard of care, resulting in an abundance of remote transmission data. While this data is valuable, the number of clinically irrelevant non-actionable alerts (NAA) can lead to alert fatigue and reduce device clinic efficiency.
Objective: We aimed to propose clinically reasonable alert parameters to reduce the number of NAA and explore its impact on clinical outcomes.
Methods: We included 412 participants with CIEDs indicated for atrial fibrillation (AF) or non-sustained ventricular tachycardia (NSVT) from a single academic medical center. Reprogramming changes set as no alerts for AF episodes < 5.5 hours, persistent AF episodes > 1 month when a prior alert has already been issued, AF episodes < 24 hours in patients with paroxysmal AF on anticoagulation or with left atrial appendage occlusion, NSVT in patients with defibrillators. The number of NAAs were tracked 90 days before and after reprogramming. Incident ischemic stroke and sudden cardiac death (SCD) was ascertained over a median follow-up of 20.9 months. Linear regression was used to compare differences in alarms between pre- and post-periods, and multivariable linear regression was applied to identify factors associated with alerts.
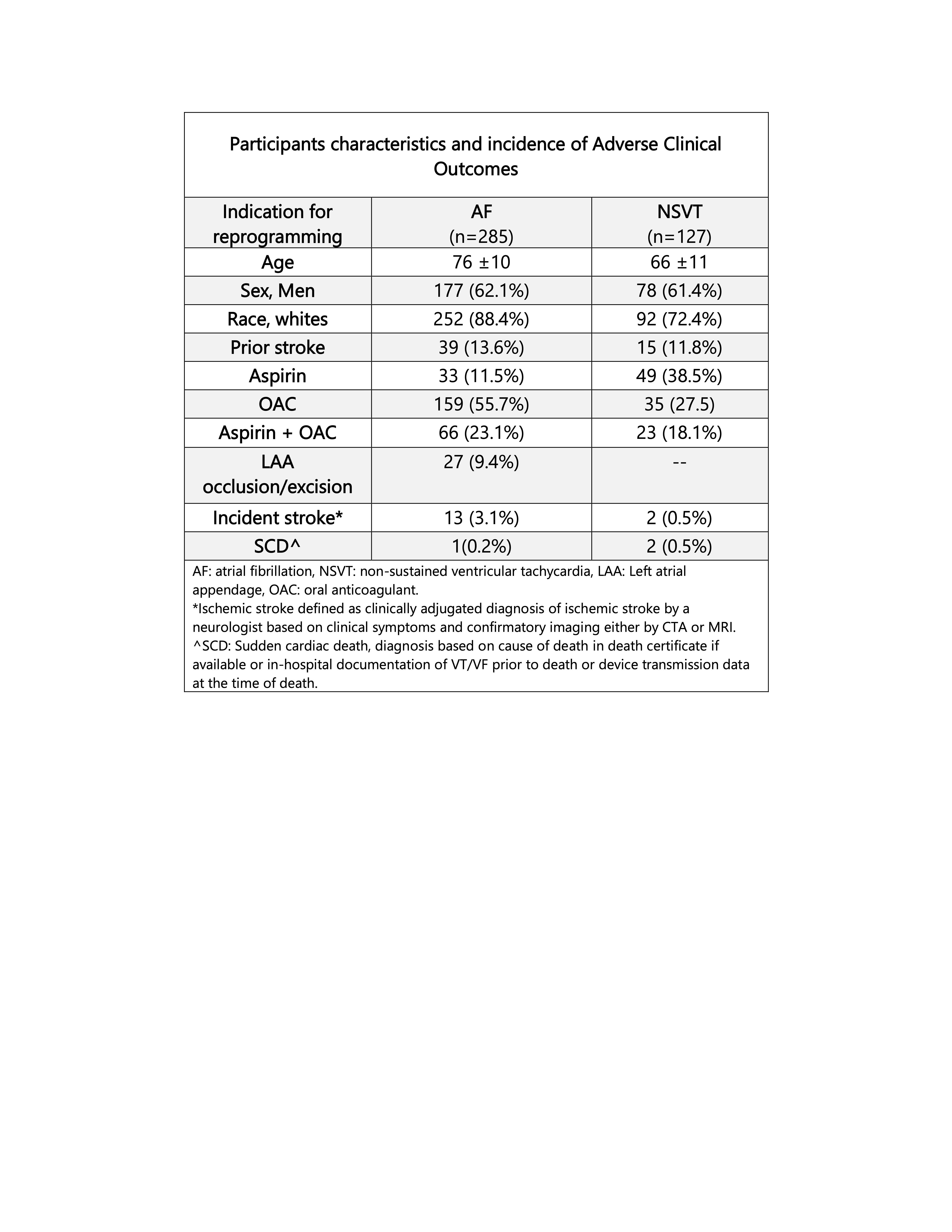
Results: Among participants, indication for reprogramming included 69% (n=285) patients with AF and 30.7% (n=127) with NSVT. Compared to pre-programming, the number of NAAs was significantly lower post reprogramming implementation (median [IQR]: 3 [6] vs. 1 [2], P < 0.001) respectively. During follow up, the incidence of primary outcomes was 3.6% (n:15) for ischemic stroke and 0.7% (n=3) for SCD. (Table)
Conclusion: Our findings demonstrate that implementing guidelines-derived alert parameters in patients with CIEDs significantly reduces the number of clinically irrelevant NAA. This reduction in NAA appears to be safe, with incidence of adverse clinical outcomes comparable to the general population of patients with CIED. This approach has the potential toreduce clinician alert fatigue and safely improve efficiency of device clinics.
Objective: We aimed to propose clinically reasonable alert parameters to reduce the number of NAA and explore its impact on clinical outcomes.
Methods: We included 412 participants with CIEDs indicated for atrial fibrillation (AF) or non-sustained ventricular tachycardia (NSVT) from a single academic medical center. Reprogramming changes set as no alerts for AF episodes < 5.5 hours, persistent AF episodes > 1 month when a prior alert has already been issued, AF episodes < 24 hours in patients with paroxysmal AF on anticoagulation or with left atrial appendage occlusion, NSVT in patients with defibrillators. The number of NAAs were tracked 90 days before and after reprogramming. Incident ischemic stroke and sudden cardiac death (SCD) was ascertained over a median follow-up of 20.9 months. Linear regression was used to compare differences in alarms between pre- and post-periods, and multivariable linear regression was applied to identify factors associated with alerts.
Results: Among participants, indication for reprogramming included 69% (n=285) patients with AF and 30.7% (n=127) with NSVT. Compared to pre-programming, the number of NAAs was significantly lower post reprogramming implementation (median [IQR]: 3 [6] vs. 1 [2], P < 0.001) respectively. During follow up, the incidence of primary outcomes was 3.6% (n:15) for ischemic stroke and 0.7% (n=3) for SCD. (Table)
Conclusion: Our findings demonstrate that implementing guidelines-derived alert parameters in patients with CIEDs significantly reduces the number of clinically irrelevant NAA. This reduction in NAA appears to be safe, with incidence of adverse clinical outcomes comparable to the general population of patients with CIED. This approach has the potential toreduce clinician alert fatigue and safely improve efficiency of device clinics.
More abstracts on this topic:
A Large Animal Model of Persistent Atrial Fibrillation
Mostafizi Pouria, Goldman Steven, Moukabary Talal, Lefkowitz Eli, Ref Jacob, Daugherty Sherry, Grijalva Adrian, Cook Kyle Eric, Chinyere Ike, Lancaster Jordan, Koevary Jen
Cardioprotective Effects of Sodium-Glucose Cotransporter-2 Inhibitors in Patients undergoingVentricular Tachycardia (VT) Ablation: A Propensity-Matched Cohort Study
Shabbir Muhammad Raffey, Osama Muhammad, Baig Ahmad Ullah, Zahra Rubab, Imtiaz Mahrukh, Sharma Param