Final ID: MDP526
Identifying Factors Influencing Response to Dual Antiplatelet Therapy in Non-Cardioembolic Ischemic Stroke and Transient Ischemic Attack: A Meta-analysis of Randomized Controlled Trials
Abstract Body (Do not enter title and authors here): Background
While dual antiplatelet therapy (DAPT) has been shown to significantly decrease recurrent stroke in patients with mild ischemic stroke or high-risk transient ischemic attack (TIA) of non-cardioembolic origin, it comes with a substantial increase in the risk of bleeding.
Research Question
Do all patients with non-cardioembolic, mild ischemic stroke/high-risk TIA derive benefits from DAPT for secondary prevention?
Aims
To identify patients who derive attenuated benefit from DAPT to avoid excessive bleeding risk.
Methods
We searched 6 databases from inception to May 10, 2024 to identify randomized-controlled trials (RCTs) comparing short-term DAPT (up to 3 months) with aspirin for secondary prevention of non-cardioembolic ischemic stroke or TIA. The primary efficacy outcome was major adverse cardiac and cerebrovascular events (MACCE), a composite of any stroke, myocardial infarction, and cardiovascular (CV) death, with prespecified subgroups based on participants’ pre-stroke treatment with statins and antiplatelet agents. Secondary efficacy outcomes comprised of recurrent ischemic events and hemorrhagic stroke. Safety outcomes included major bleeding, CV mortality, and all-cause mortality. A random-effects meta-analysis was performed using restricted maximum likelihood method.
Results
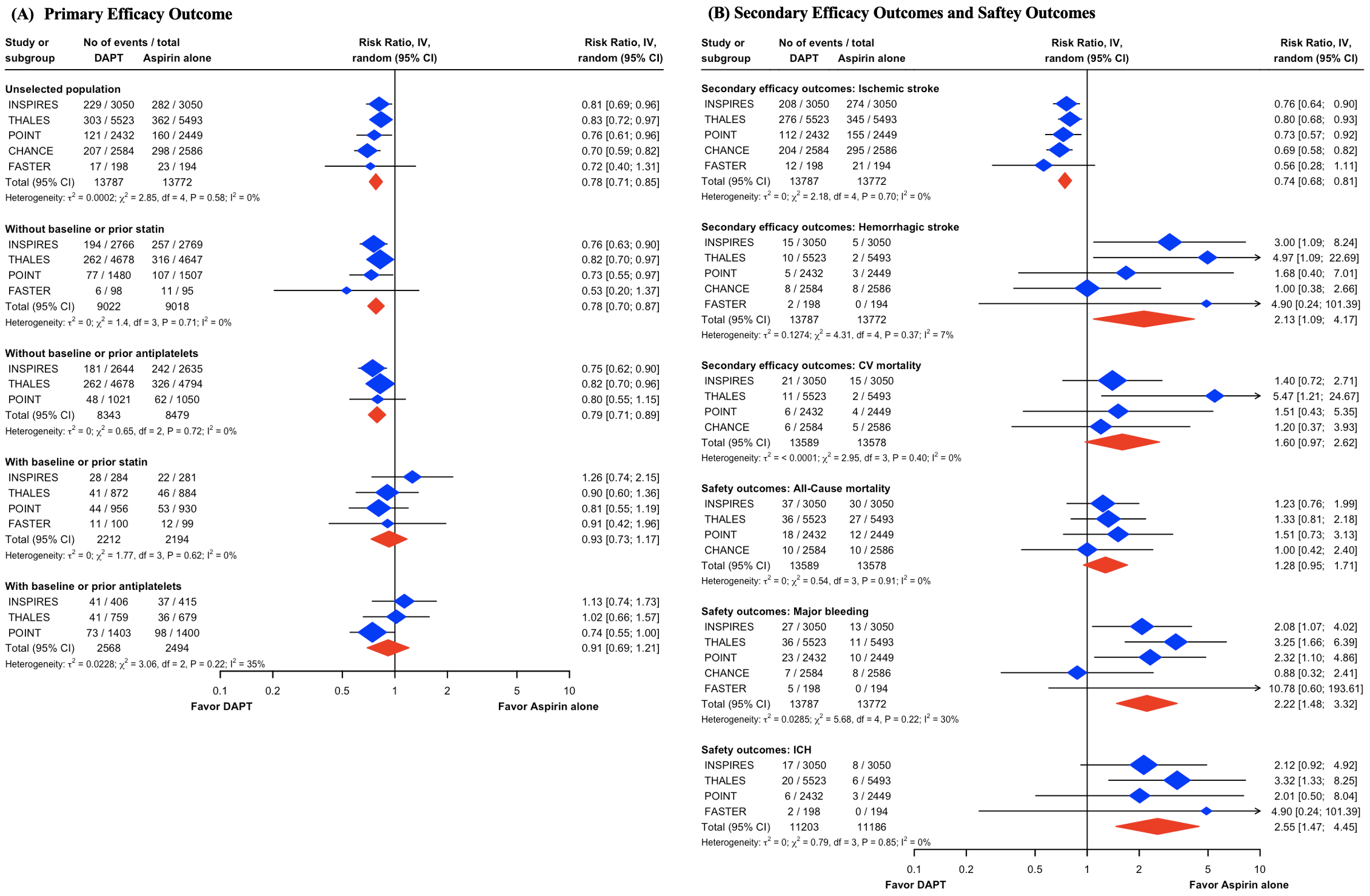
There were 5 RCTs including 27,559 patients. In the unselected population, DAPT significantly reduced MACCE (RR, 0.78; 95% CI, 0.71 to 0.85; I2 = 0%; Figure 1A), compared to aspirin. However, patients with baseline statin (RR, 0.93; 95% CI, 0.73 to 1.17; I2 = 0%; Figure 1A) or antiplatelet (RR, 0.91; 95% CI, 0.69 to 1.21; I2 = 0%; Figure 1A) before index events did not derive benefits from DAPT. While DAPT led to significantly lower recurrent ischemic stroke (RR, 0.74; 95% CI, 0.68 to 0.81; I2 = 0%; Figure 1B), it resulted in a significantly higher risk of hemorrhagic stroke, major bleeding, and intracerebral hemorrhage, compared to aspirin (Figure 1B). Moreover, the use of DAPT trended toward an increased risk of all-cause and CV mortality (Figure 1B).
Conclusions
Patients with baseline statin/antiplatelts use may not derive the same benefits from DAPT for secondary prevention of non-cardioembolic ischemic stroke or TIA.
While dual antiplatelet therapy (DAPT) has been shown to significantly decrease recurrent stroke in patients with mild ischemic stroke or high-risk transient ischemic attack (TIA) of non-cardioembolic origin, it comes with a substantial increase in the risk of bleeding.
Research Question
Do all patients with non-cardioembolic, mild ischemic stroke/high-risk TIA derive benefits from DAPT for secondary prevention?
Aims
To identify patients who derive attenuated benefit from DAPT to avoid excessive bleeding risk.
Methods
We searched 6 databases from inception to May 10, 2024 to identify randomized-controlled trials (RCTs) comparing short-term DAPT (up to 3 months) with aspirin for secondary prevention of non-cardioembolic ischemic stroke or TIA. The primary efficacy outcome was major adverse cardiac and cerebrovascular events (MACCE), a composite of any stroke, myocardial infarction, and cardiovascular (CV) death, with prespecified subgroups based on participants’ pre-stroke treatment with statins and antiplatelet agents. Secondary efficacy outcomes comprised of recurrent ischemic events and hemorrhagic stroke. Safety outcomes included major bleeding, CV mortality, and all-cause mortality. A random-effects meta-analysis was performed using restricted maximum likelihood method.
Results
There were 5 RCTs including 27,559 patients. In the unselected population, DAPT significantly reduced MACCE (RR, 0.78; 95% CI, 0.71 to 0.85; I2 = 0%; Figure 1A), compared to aspirin. However, patients with baseline statin (RR, 0.93; 95% CI, 0.73 to 1.17; I2 = 0%; Figure 1A) or antiplatelet (RR, 0.91; 95% CI, 0.69 to 1.21; I2 = 0%; Figure 1A) before index events did not derive benefits from DAPT. While DAPT led to significantly lower recurrent ischemic stroke (RR, 0.74; 95% CI, 0.68 to 0.81; I2 = 0%; Figure 1B), it resulted in a significantly higher risk of hemorrhagic stroke, major bleeding, and intracerebral hemorrhage, compared to aspirin (Figure 1B). Moreover, the use of DAPT trended toward an increased risk of all-cause and CV mortality (Figure 1B).
Conclusions
Patients with baseline statin/antiplatelts use may not derive the same benefits from DAPT for secondary prevention of non-cardioembolic ischemic stroke or TIA.
More abstracts on this topic:
A First-in-Class Humanized Antibody Fragment Targeting Platelet Glycoprotein Ibα: A Comprehensive Preclinical Study of CA1001 for the Treatment of Acute Ischemic Stroke
Xu Xiaohong, Preeti Preeti, Yu Ruoying, Shaykhalishahi Hamed, Zhang Cheng, Shen Chuanbin, Li Bei, Tang Naping, Chang Yan, Xiang Qian, Cui Yimin, Lei Xi, Ni Heyu, Zhu Guangheng, Liu Zhenze, Hu Xudong, Slavkovic Sladjana, Neves Miguel, Ma Wenjing, Xie Huifang
10-Year Trend Analysis of Medicare Payment in Stroke Inpatient Hospital AdmissionWong Ka-ho, Krothapalli Neeharika, Littig Lauren, Champagne Alison, Majersik Jennifer, Reddy Vivek, De Havenon Adam