Final ID: Mo4009
Comparative Bleeding Risks Following Acute Myocardial Infarction: Clopidogrel and Ticagrelor, with Consideration for Clopidogrel Resistance
Abstract Body (Do not enter title and authors here): Various studies have shown higher bleeding risks with ticagrelor in comparison to clopidogrel in acute myocardial infarction (AMI). The literature also reveals significant variability in Clopidogrel resistance and consequent efficacy in patients. Our study compares the post-AMI bleeding risks and outcomes of patients on Clopidogrel with confirmed inhibition of platelet aggregation via P2Y12 platelet reactivity assay, compared to Ticagrelor.
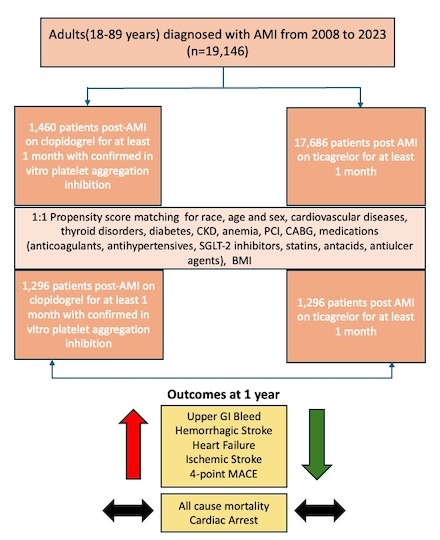
We queried the TriNeTX Global collaborative network for adults diagnosed with AMI between 01/01/08 to 12/31/23 and created two cohorts: one on Clopidogrel for at least one month post-AMI, after confirmed ADP-mediated P2Y12 inhibitor effect, and the second cohort was on Ticagrelor for at least one month post-AMI. We conducted propensity score matching(PSM) for around 35 variables, including race, age, sex, medications, and other comorbidities. Logistic regression was used to calculate the odds ratios (OR) and 95% confidence intervals (CI) at one year. Upper Gastrointestinal (GI) bleeding and hemorrhagic stroke at one year were the primary outcomes. Secondary outcomes included 4-point major adverse cardiovascular and cerebrovascular events (MACCE) defined as a composite of all-cause mortality, cardiac arrest, heart failure, and ischemic stroke.
The sample population had 1,460 post-AMI patients in the Clopidogrel cohort (Cohort 1) and 17,686 post-AMI patients on Ticagrelor (Cohort 2). After PSM both cohorts had 1,296 patients. The Clopidogrel cohort had significantly increased odds of upper GI bleeding (OR 1.656, 95% CI, 1.092-2.511) and hemorrhagic stroke (OR 2.119, 95% CI, 1.110 - 4.044) compared to Cohort 2 at one year. Among secondary outcomes, there was increased odds of heart failure (OR 1.565, 95%CI, 1.118-2.190), ischemic stroke (OR 1.745, 95%CI, 1.098 - 2.775), and 4-point MACCE (OR 1.549, 95%CI, 1.110 - 2.160) in the clopidogrel group compared to ticagrelor. There was no significance noticed in cardiac arrest and all cause-mortality.
In our study, post-AMI patients on Clopidogrel with confirmed in-vitro platelet aggregation effect had significantly higher odds of bleeding and MACCE than those on Ticagrelor. However, Ticagrelor use did not show any mortality benefit.
We queried the TriNeTX Global collaborative network for adults diagnosed with AMI between 01/01/08 to 12/31/23 and created two cohorts: one on Clopidogrel for at least one month post-AMI, after confirmed ADP-mediated P2Y12 inhibitor effect, and the second cohort was on Ticagrelor for at least one month post-AMI. We conducted propensity score matching(PSM) for around 35 variables, including race, age, sex, medications, and other comorbidities. Logistic regression was used to calculate the odds ratios (OR) and 95% confidence intervals (CI) at one year. Upper Gastrointestinal (GI) bleeding and hemorrhagic stroke at one year were the primary outcomes. Secondary outcomes included 4-point major adverse cardiovascular and cerebrovascular events (MACCE) defined as a composite of all-cause mortality, cardiac arrest, heart failure, and ischemic stroke.
The sample population had 1,460 post-AMI patients in the Clopidogrel cohort (Cohort 1) and 17,686 post-AMI patients on Ticagrelor (Cohort 2). After PSM both cohorts had 1,296 patients. The Clopidogrel cohort had significantly increased odds of upper GI bleeding (OR 1.656, 95% CI, 1.092-2.511) and hemorrhagic stroke (OR 2.119, 95% CI, 1.110 - 4.044) compared to Cohort 2 at one year. Among secondary outcomes, there was increased odds of heart failure (OR 1.565, 95%CI, 1.118-2.190), ischemic stroke (OR 1.745, 95%CI, 1.098 - 2.775), and 4-point MACCE (OR 1.549, 95%CI, 1.110 - 2.160) in the clopidogrel group compared to ticagrelor. There was no significance noticed in cardiac arrest and all cause-mortality.
In our study, post-AMI patients on Clopidogrel with confirmed in-vitro platelet aggregation effect had significantly higher odds of bleeding and MACCE than those on Ticagrelor. However, Ticagrelor use did not show any mortality benefit.
More abstracts on this topic:
A New Small-Molecule ErbB4 Agonist Attenuates Adverse Ventricular Remodeling After Myocardial Infarction In a Sex-Specific Manner
Goovaerts Bo, Civati Celine, Feyen Eline, De Keulenaer Gilles, Segers Vincent
A Randomized Clinical Trial Evaluating Vitamin D Normalization on Major Adverse Cardiovascular-Related Events Among Acute Coronary Syndrome Patients: The TARGET-D TrialMay Heidi, Colipi Dominique, Whiting Tyler, Muhlestein Joseph, Le Viet, Anderson Jeffrey, Babcock Daniel, Wayman Libby, Bair Tami, Knight Stacey, Knowlton Kirk, Iverson Leslie