Final ID: Su2193
The Prognostic Role of Glucagon-like Peptide-1 Receptor Agonist in Transthyretin Amyloid Cardiomyopathy
Abstract Body (Do not enter title and authors here): Background
Guideline-directed medical therapy (GDMTs) for heart failure is often poorly tolerated in patients with transthyretin amyloid cardiomyopathy (ATTR-CM) and has unclear efficacy. Contrasting with GDMTs, glucagon-like peptide-1 receptor agonist (GLP1a) does not affect cardiovascular hemodynamics in patients with restrictive physiology.
Research Question
What is the association between GLP1a treatment and survival outcomes in patients with ATTR-CM?
Aims
To examine the prognostic role of GLP1a in patients with ATTR-CM.
Methods
We used the TriNetX Global Collaborative Network database to conduct a retrospective propensity-score matching (PSM) study including adult patients with ATTR-CM, identified through tafamidis records, between September 1, 2019, and January 1, 2024. GLP1a users were defined as those having at least one prescription for GLP1a after the first dispense of tafamidis. GLP1a non-users were those who had no GLP1a prescription in the database but had at least one ambulatory visit after the first tafamidis prescription. The index date for study follow-up was set as the first GLP1a dispense for users and the first ambulatory visit after the first tafamidis prescription for non-users. The primary endpoint was heart failure (HF) hospitalization. The secondary endpoint was all-cause mortality. Incident gastrointestinal bleeding was set as a falsification endpoint. Cox proportional hazard ratios (HR) were calculated to compare study endpoints occurring within two years of the index date between two arms.
Results
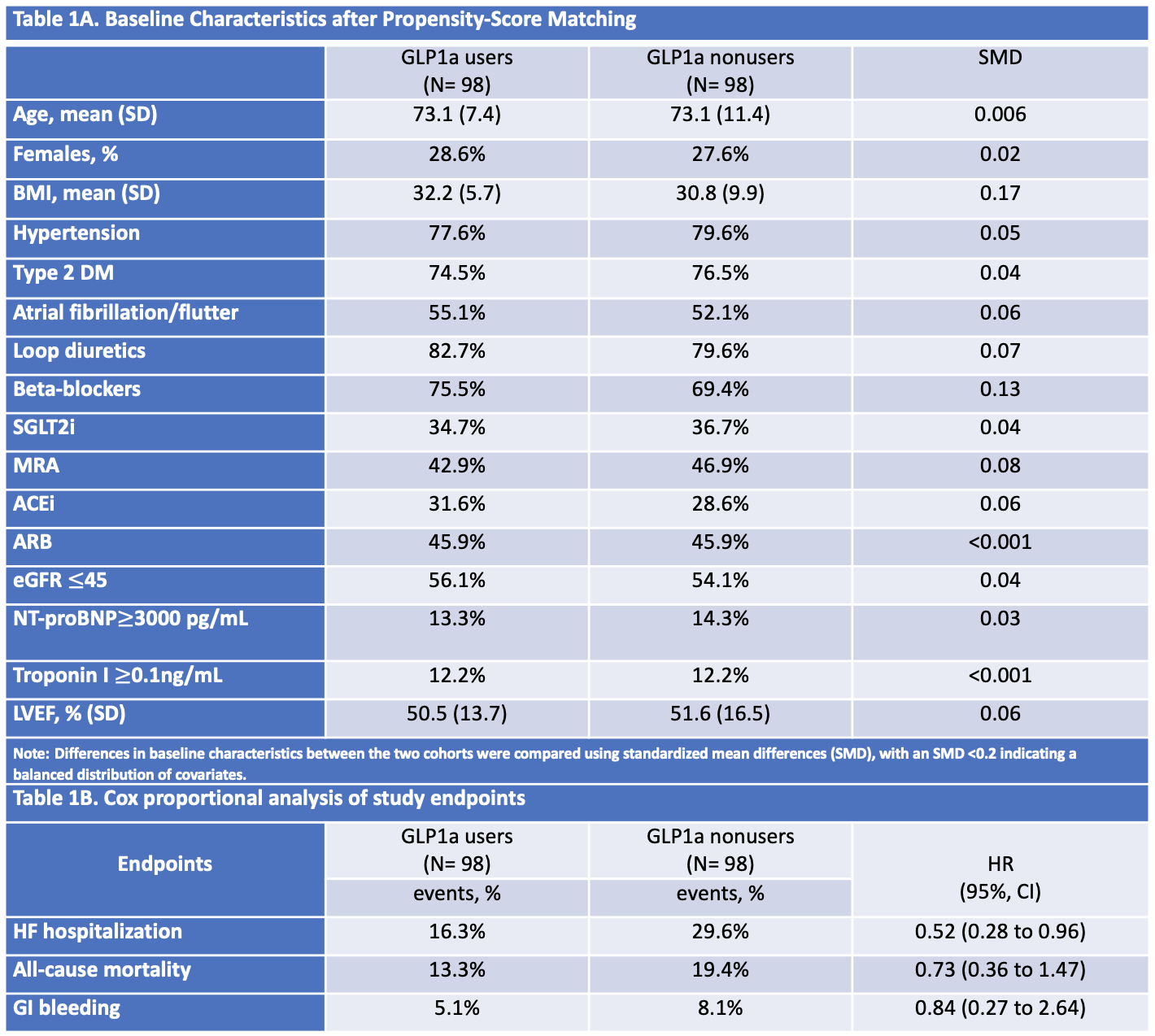
Of 5,241 ATTR-CM patients treated with tafamidis, 98 GLP1a users were matched to 98 nonusers. Before PSM, the mean BMI (33.4 vs 27.1) and the prevalence of type 2 diabetes (79.0% vs 19.0%) were higher in GLP1a users. After PSM, key covariates were balanced between the two cohorts (Table 1A). The use of GLP1a was associated with a significant reduction in HF hospitalization (HR, 95% CI, 0.52; 0.28 to 0.96) (Table 1B), compared with non-users. There was no significant difference in all-cause mortality (HR, 95% CI, 0.73; 0.36 to 1.47) and the falsification endpoint between the two groups (Table 1B).
Conclusions
In ATTR-CM, GLP1a use was associated with a significant reduction in HF hospitalization.
Guideline-directed medical therapy (GDMTs) for heart failure is often poorly tolerated in patients with transthyretin amyloid cardiomyopathy (ATTR-CM) and has unclear efficacy. Contrasting with GDMTs, glucagon-like peptide-1 receptor agonist (GLP1a) does not affect cardiovascular hemodynamics in patients with restrictive physiology.
Research Question
What is the association between GLP1a treatment and survival outcomes in patients with ATTR-CM?
Aims
To examine the prognostic role of GLP1a in patients with ATTR-CM.
Methods
We used the TriNetX Global Collaborative Network database to conduct a retrospective propensity-score matching (PSM) study including adult patients with ATTR-CM, identified through tafamidis records, between September 1, 2019, and January 1, 2024. GLP1a users were defined as those having at least one prescription for GLP1a after the first dispense of tafamidis. GLP1a non-users were those who had no GLP1a prescription in the database but had at least one ambulatory visit after the first tafamidis prescription. The index date for study follow-up was set as the first GLP1a dispense for users and the first ambulatory visit after the first tafamidis prescription for non-users. The primary endpoint was heart failure (HF) hospitalization. The secondary endpoint was all-cause mortality. Incident gastrointestinal bleeding was set as a falsification endpoint. Cox proportional hazard ratios (HR) were calculated to compare study endpoints occurring within two years of the index date between two arms.
Results
Of 5,241 ATTR-CM patients treated with tafamidis, 98 GLP1a users were matched to 98 nonusers. Before PSM, the mean BMI (33.4 vs 27.1) and the prevalence of type 2 diabetes (79.0% vs 19.0%) were higher in GLP1a users. After PSM, key covariates were balanced between the two cohorts (Table 1A). The use of GLP1a was associated with a significant reduction in HF hospitalization (HR, 95% CI, 0.52; 0.28 to 0.96) (Table 1B), compared with non-users. There was no significant difference in all-cause mortality (HR, 95% CI, 0.73; 0.36 to 1.47) and the falsification endpoint between the two groups (Table 1B).
Conclusions
In ATTR-CM, GLP1a use was associated with a significant reduction in HF hospitalization.
More abstracts on this topic:
Add-on Therapy with Dantrolene, a RyR2 Stabilizer, Terminates Ventricular Tachycardia Storm refractory to Intravenous Amiodarone in Heart Failure.
Nawata Junya, Omuro Ayumi, Fukuda Masakazu, Suetomi Takeshi, Miyazaki Yosuke, Fujimura Tatsuhiro, Mochizuki Mamoru, Sano Motoaki, Kobayashi Shigeki, Ishikawa Maho, Nakata Yuki, Murakawa Kaori, Nakashima Yusuke, Hisaoka Masahiro, Matsuyama Tetsuya, Nakamura Yoshihide
5-oxoproline/ OPLAH Axis Alleviates Doxorubicin-induced Cardiomyopathy By Inhibiting FerroptosisJiang Meng, Guo Xinning