Final ID: MDP394
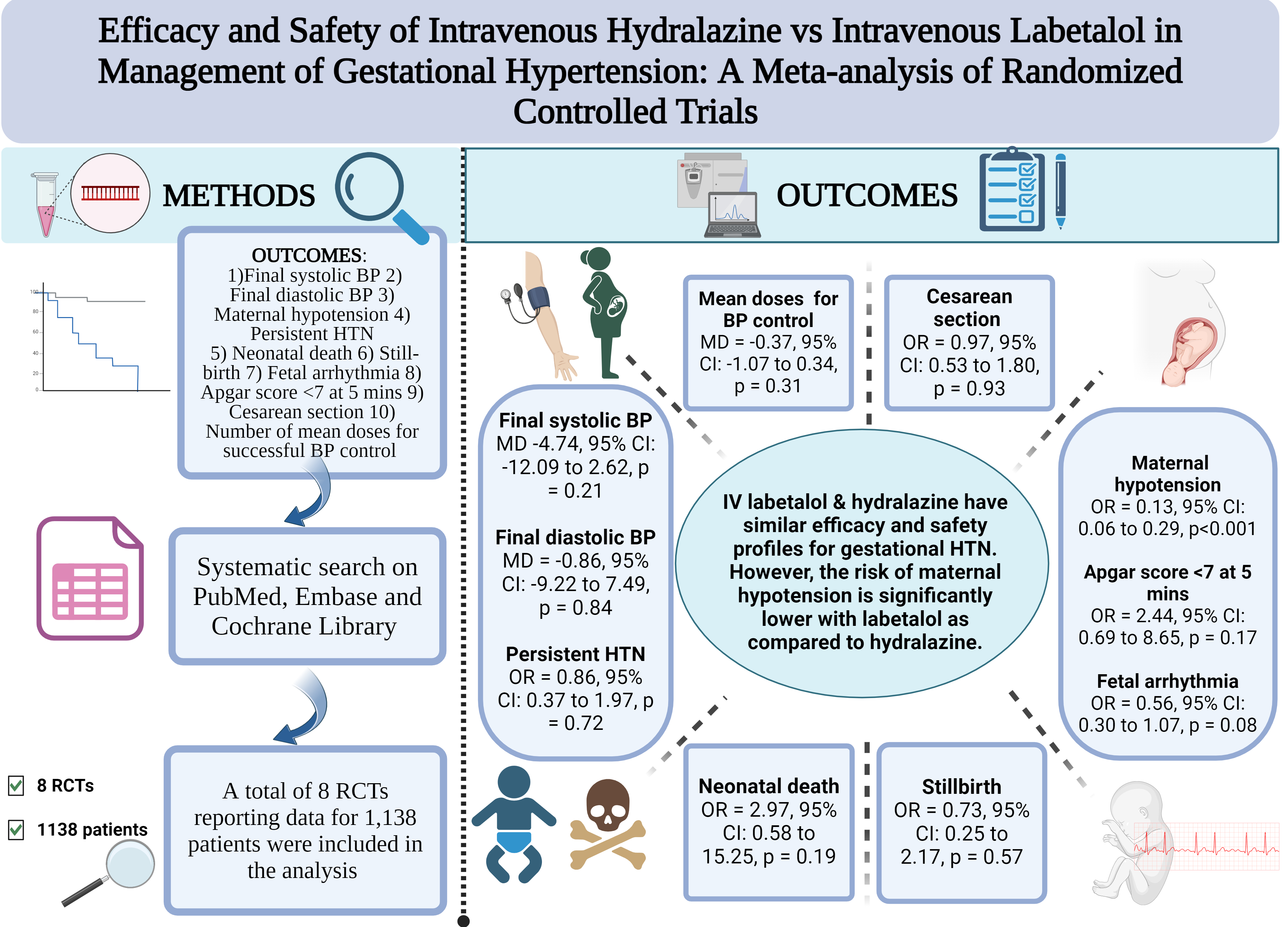
Efficacy and Safety of Intravenous Hydralazine vs Intravenous Labetalol in Management of Gestational Hypertension: A Meta-analysis of Randomized Controlled Trials
Abstract Body (Do not enter title and authors here): Background
Hypertension in pregnancy affects around 15% of all pregnant women and is one of the leading causes of maternal and fetal, mortality and morbidity. Hydralazine and labetalol are administered intravenously to control hypertension in pregnant women. However, data regarding their comparative efficacy and safety is limited. Considering the paucity of data, we conducted a systematic review and meta-analysis to pool all the studies published on this subject and provide robust evidence.
Methods
We followed PRISMA guidelines for conducting this systematic review and meta-analysis. Two investigators searched PubMed/MEDLINE, Scopus, the Cochrane Library, and Google Scholar from inception until May 2024. The randomized controlled trials (RCTs) which compared the effects of intravenous labetalol versus hydralazine in pregnant women with hypertensive disorder of pregnancy were included in our pooled analysis. A random-effects model was used to calculate the weighted mean differences (MD) for continuous outcomes and odds ratio (OR) for the discrete outcomes along with the corresponding 95% confidence intervals (CIs). We considered a p-value of less than 0.05 statistically significant in all cases.
Results
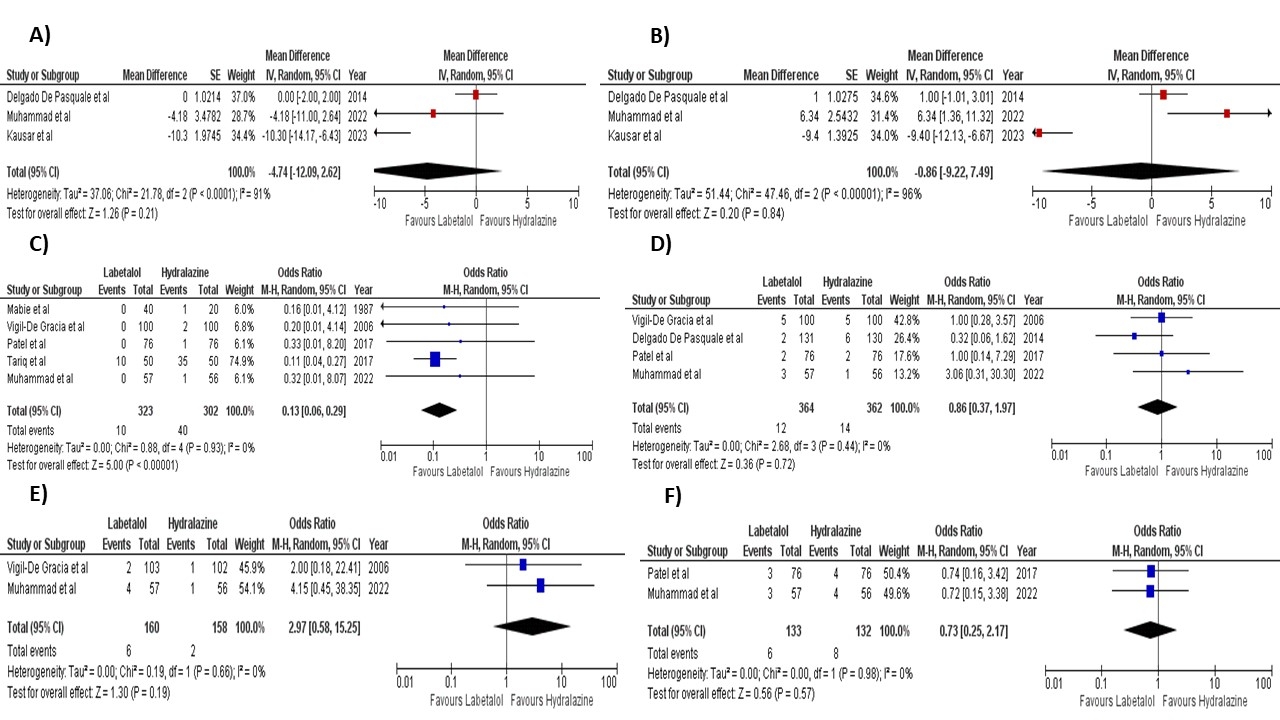
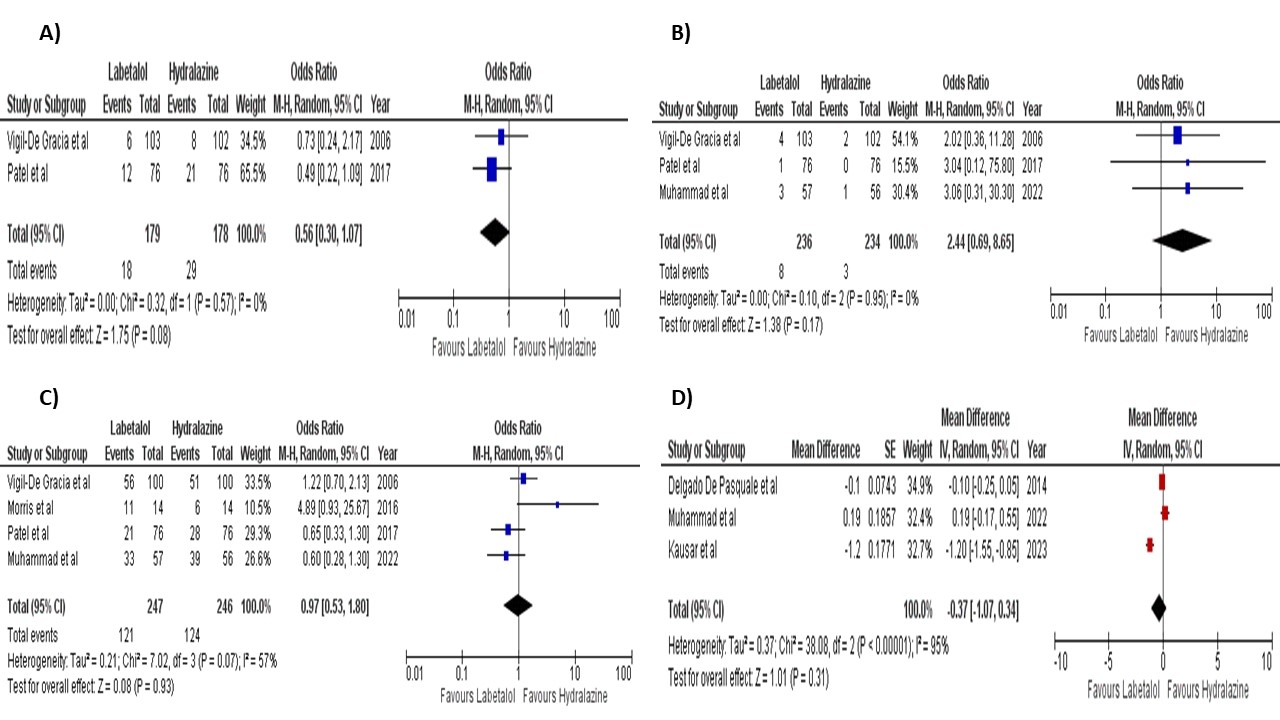
A total of 8 RCTs with total population of 1138 patients were pooled. The pooled analysis showed that the final systolic blood pressure (MD = -4.74, 95% CI: -12.09 to 2.62, p = 0.21) and diastolic pressure (MD = -0.86, 95% CI: -9.22 to 7.49, p = 0.84) remained comparable. The incidence of maternal hypotension (OR = 0.13, 95% CI: 0.06 to 0.29, p<0.001) was significantly lower with labetalol administration compared to hydralazine. However, we found no statistically significant difference between two groups for persistent hypertension (OR = 0.86, 95% CI: 0.37 to 1.97, p = 0.72), neonatal death (OR = 2.97, 95% CI: 0.58 to 15.25, p = 0.19), stillbirth (OR = 0.73, 95% CI: 0.25 to 2.17, p = 0.57), fetal arrhythmia (OR = 0.56, 95% CI: 0.30 to 1.07, p = 0.08), APGAR score < 7 at 5 min (OR = 2.44, 95% CI: 0.69 to 8.65, p = 0.17), cesarean section (OR = 0.97, 95% CI: 0.53 to 1.80, p = 0.93), and the number of mean doses required for successful blood pressure control (MD = -0.37, 95% CI: -1.07 to 0.34, p = 0.31).
Conclusion
Intravenous labetalol and hydralazine have similar efficacy and safety profiles for blood pressure control in pregnant women. However, the risk of maternal hypotension is significantly lower with labetalol administration as compared to hydralazine.
Hypertension in pregnancy affects around 15% of all pregnant women and is one of the leading causes of maternal and fetal, mortality and morbidity. Hydralazine and labetalol are administered intravenously to control hypertension in pregnant women. However, data regarding their comparative efficacy and safety is limited. Considering the paucity of data, we conducted a systematic review and meta-analysis to pool all the studies published on this subject and provide robust evidence.
Methods
We followed PRISMA guidelines for conducting this systematic review and meta-analysis. Two investigators searched PubMed/MEDLINE, Scopus, the Cochrane Library, and Google Scholar from inception until May 2024. The randomized controlled trials (RCTs) which compared the effects of intravenous labetalol versus hydralazine in pregnant women with hypertensive disorder of pregnancy were included in our pooled analysis. A random-effects model was used to calculate the weighted mean differences (MD) for continuous outcomes and odds ratio (OR) for the discrete outcomes along with the corresponding 95% confidence intervals (CIs). We considered a p-value of less than 0.05 statistically significant in all cases.
Results
A total of 8 RCTs with total population of 1138 patients were pooled. The pooled analysis showed that the final systolic blood pressure (MD = -4.74, 95% CI: -12.09 to 2.62, p = 0.21) and diastolic pressure (MD = -0.86, 95% CI: -9.22 to 7.49, p = 0.84) remained comparable. The incidence of maternal hypotension (OR = 0.13, 95% CI: 0.06 to 0.29, p<0.001) was significantly lower with labetalol administration compared to hydralazine. However, we found no statistically significant difference between two groups for persistent hypertension (OR = 0.86, 95% CI: 0.37 to 1.97, p = 0.72), neonatal death (OR = 2.97, 95% CI: 0.58 to 15.25, p = 0.19), stillbirth (OR = 0.73, 95% CI: 0.25 to 2.17, p = 0.57), fetal arrhythmia (OR = 0.56, 95% CI: 0.30 to 1.07, p = 0.08), APGAR score < 7 at 5 min (OR = 2.44, 95% CI: 0.69 to 8.65, p = 0.17), cesarean section (OR = 0.97, 95% CI: 0.53 to 1.80, p = 0.93), and the number of mean doses required for successful blood pressure control (MD = -0.37, 95% CI: -1.07 to 0.34, p = 0.31).
Conclusion
Intravenous labetalol and hydralazine have similar efficacy and safety profiles for blood pressure control in pregnant women. However, the risk of maternal hypotension is significantly lower with labetalol administration as compared to hydralazine.
More abstracts on this topic:
APOL1 Risk Variants in Preeclampsia: From Mechanistic Insights to Therapeutic Opportunities
Rao Vivikta, Waikar Sushrut, Wei Jin, Fu Jiayi, Liaw Easton, De Thea, Sedarski Jonathan, Tang Janice, Zhang Jie, Kuohung Wendy, Ilori Titilayo
Endothelial Susceptibility-Related Genetic Variants and Hypertensive Disorders of PregnancyLi Linke, Zhang Yu, Truong Buu, Yu Zhi, Marston Nicholas, Gupta Rajat, Haas David, Liu Nianjun, Honigberg Michael