Final ID: 48
Cardiovascular Health Modifies Genetic Risk for the Hypertensive Disorders of Pregnancy
Hypertensive disorders of pregnancy (HDP) are a leading cause of maternal/perinatal mortality. In recent work, a genetic risk score improved prediction of HDPs beyond standard clinical risk factors, but the extent to which cardiovascular health (CVH) modifies HDP genetic risk is unknown.
Hypothesis:
First-trimester CVH can offset genetic risk for HDPs.
Methods:
We examined genotyped participants of the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-To-Be (nuMoM2b). Individual HDP genetic risk was calculated using a validated polygenic score. A composite first-trimester CVH score was adapted from the Life’s Essential 8 model; cholesterol was incorporated in a subset (47%) with available first-trimester values. Genetic risk and CVH were each grouped as low (bottom quintile), intermediate (Q2-4), and high (top quintile). Logistic regression tested the joint association of CVH and genetic risk with HDP, adjusted for age and sociodemographic covariates.
Results:
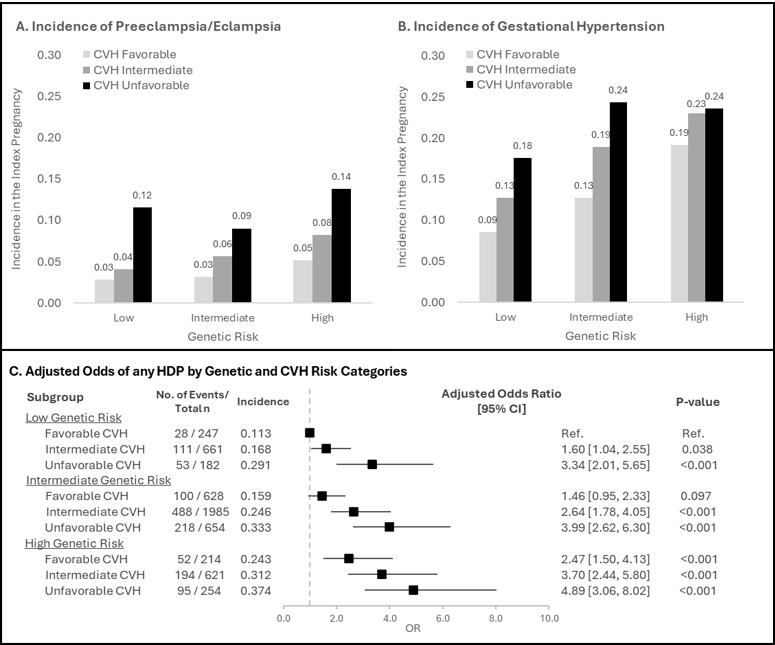
Among 5,446 participants (mean age 27.5 years), 1,339 (24.6%) developed HDP (344 [6.3%] preeclampsia, 995 [18.3%] gestational hypertension [GH]). Higher genetic risk and lower CVH were additively associated with risk of HDP (Figure 1A-B) with no significant interaction (P[interaction] >0.05). HDP incidence ranged from 11% (low genetic risk, favorable CVH) to 37% (high genetic risk, unfavorable CVH) (Figure 1C). Favorable vs. unfavorable CVH was associated with 35-62% lower risk of HDPs across genetic risk groups. Findings were broadly consistent when examining preeclampsia and GH separately and when incorporating cholesterol (i.e., using a complete Life’s Essential 8 score). Among CVH components, nonideal BMI, blood pressure, and diet conferred highest population attributable HDP risk (25%, 14%, and 12%, respectively).
Conclusion:
Higher genetic risk and lower first trimester CVH were additively associated with risk of developing HDP. Favorable CVH in early pregnancy may partially offset a higher genetic risk for HDP.
- Mathew, Vineetha ( Broad Institute of MIT and Harvard , Boston , Massachusetts , United States )
- Patel, Aniruddh ( Massachusetts General Hospital , Brookline , Massachusetts , United States )
- Cho, So Mi ( Broad Institute of MIT and Harvard , Boston , Massachusetts , United States )
- Jowell, Amanda ( Harvard Medical School , Brookline , Massachusetts , United States )
- Pabon, Maria ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Silver, Robert ( University of Utah , Salt Lake City , Utah , United States )
- Levine, Lisa ( University of Pennsylvania , Philadelphia , Pennsylvania , United States )
- Grobman, William ( The Ohio State University Medical Center , Tulsa , Oklahoma , United States )
- Catov, Janet ( UNIVERSITY OF PITTSBURGH , Pittsburgh , Pennsylvania , United States )
- Haas, David ( Indiana University School of Medicine , Indianapolis , Indiana , United States )
- Honigberg, Michael ( Massachusetts General Hospital , Brookline , Massachusetts , United States )
- Khan, Raiyan ( Columbia University , New York , New York , United States )
- Mcneil, Rebecca ( RTI International , Durham , North Carolina , United States )
- Yan, Qi ( Columbia University , New York , New York , United States )
- Pe Er, Itsik ( Columbia University , New York , New York , United States )
- Truong, Buu ( Broad Institute of MIT and Harvard , Boston , Massachusetts , United States )
- Natarajan, Pradeep ( Massachusetts General Hospital , Brookline , Massachusetts , United States )
- Yee, Lynn ( Northwestern , Chicago , Illinois , United States )
- Sharma, Garima ( Inova Fairfax Medical Campus , Falls Church , Virginia , United States )
Meeting Info:
Session Info:
18.A TAC Oral Abstract Award Competition
Saturday, 09/07/2024 , 01:30PM - 03:00PM
Oral Abstract TAC Award
More abstracts on this topic:
Chen Victoria, William Jeffrey, Venkataraman Shilpa, Triot Alexa, Cluett Jennifer
Gestational Hypertension in the Latine Population by Race, Ancestry, and Nativity: An Intersectional-MAIHDA ApproachCisneros Marissa
More abstracts from these authors:
Shree Raj, Bairey Merz C Noel, Grobman William, Catov Janet, Pike Mindy, Simhan Hyagriv, Yee Lynn, Levine Lisa, Silver Robert, Hoffman Matthew, Greenland Philip, Saade George
Racial Disparities in Low-Density Lipoprotein Cholesterol Control and Lipoprotein(a) Testing Among Young Adult Women with Severe HyperlipidemiaJowell Amanda, Cho So Mi, Faaborg-andersen Christian, Yu Zhi, Natarajan Pradeep, Honigberg Michael, Harrington Colleen