Final ID: MDP1803
Quantitative Testing Reveals Severity of Autonomic Dysfunction after Acute COVID-19 Infection: A Comparison with Controls and Autonomic Failure
Abstract Body (Do not enter title and authors here): Background: COVID-19 infections have been associated with cardiovascular autonomic dysfunction (AD). Clinical findings include fatigue, cognitive impairment, and postural intolerance. However, quantitative post-COVID AD assessments are lacking.
Objective: Compare autonomic testing measures of post-COVID-19 subjects to controls and those with pure autonomic failure (PAF).
Methods: Autonomic testing included 1) change in heart rate (HR) and blood pressure (BP) with active standing (AS) and tilt table testing (TT), 2) time to BP nadir and recovery during AS and TT, 3) Valsalva ratio (VR), and 4) respiratory sinus arrhythmia (RSA). Comparisons between two groups were made using t-tests, Kruskal-Wallis, or chi-square tests. Multivariable linear regression was used to adjust findings for age and sex. A p-value of <0.05 was considered significant.
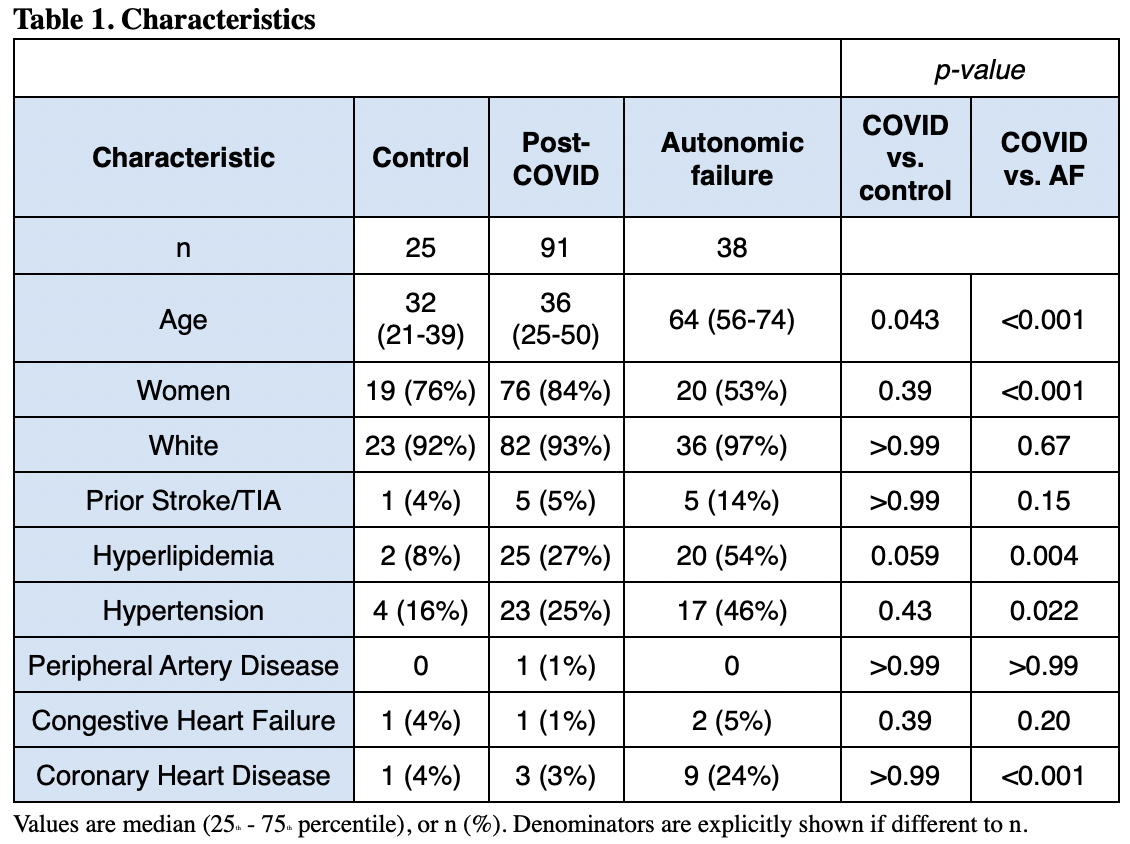
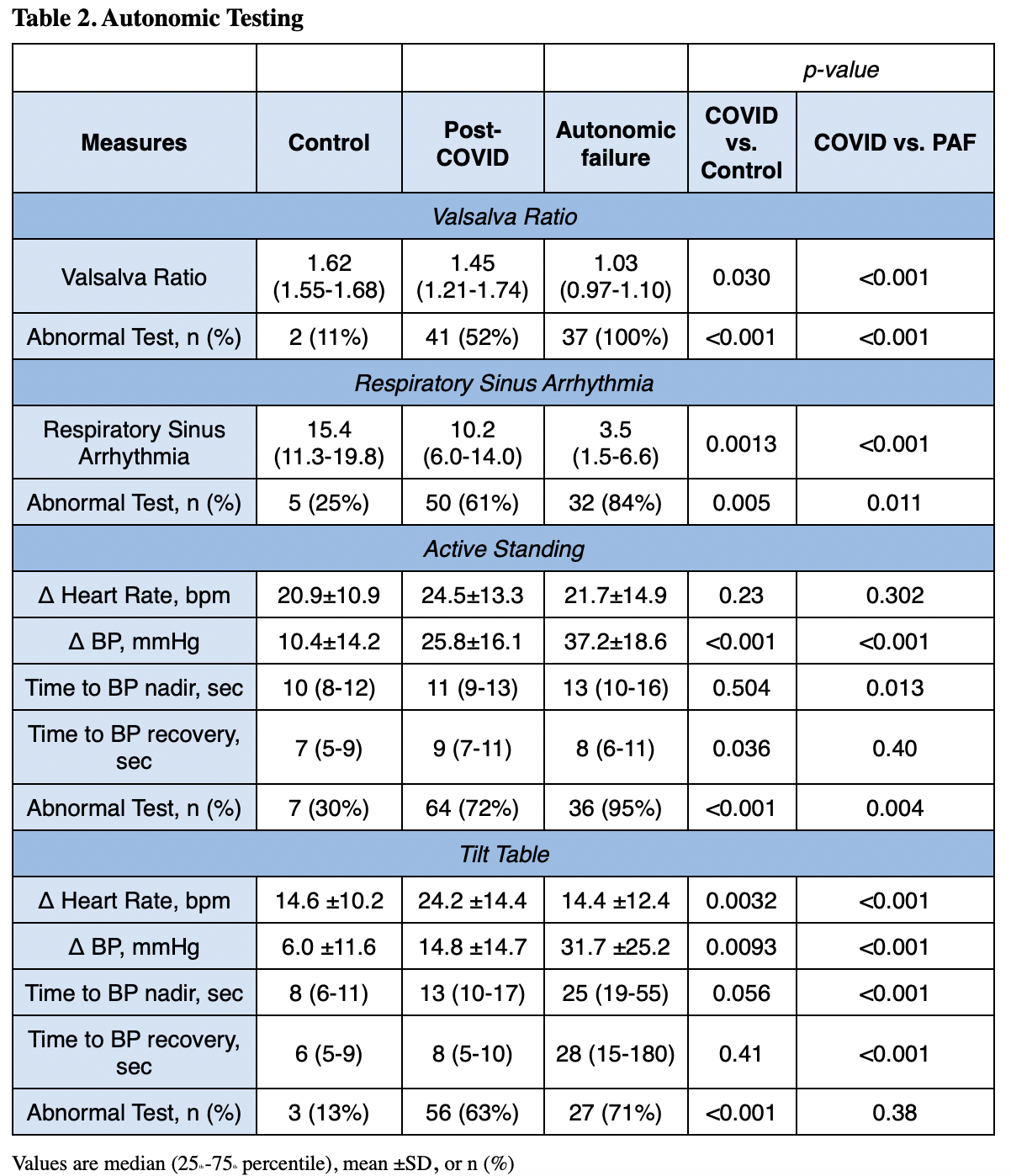
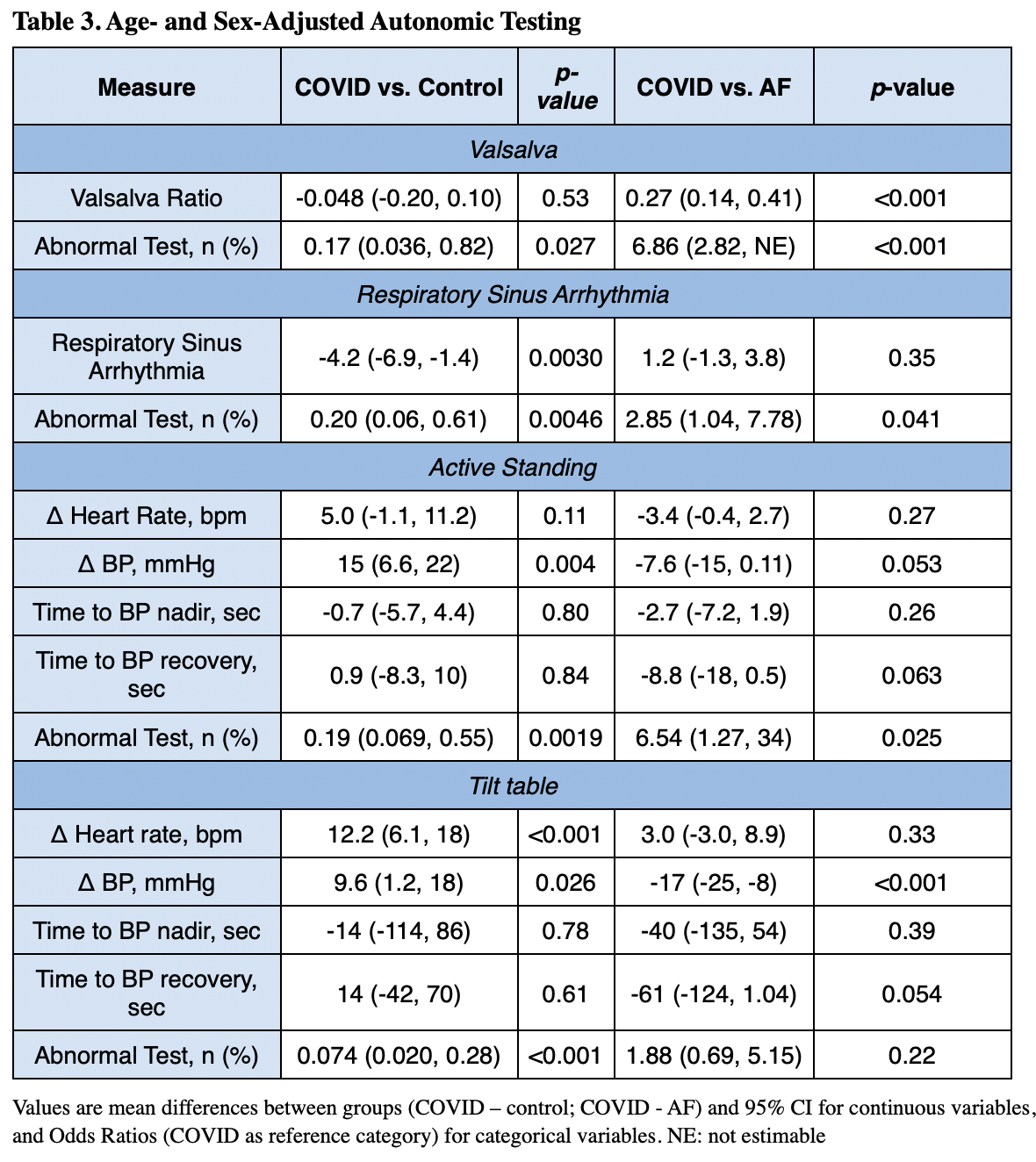
Results: Control subjects (n=25, median 32 [21-39] years, 76% female) and post-COVID patients (n=91, median 36 [25-50] years, 84% female, mean 11.96 [±9.14] months from infection) were similar in age and sex, while the PAF group (n=38, median 64 [56-74] years, 53% female) was older and comprised of more males (Table 1). The VR and RSA of the post-COVID group was significantly lower than controls, but higher than the PAF group (Table 2). The change in BP with AS and TT for post-COVID subjects was significantly higher than controls and lower than the PAF group. The post-COVID group also had a significantly increased change in HR with TT compared to both the control and PAF groups. Across all four tests, the post-COVID group had a higher proportion of abnormal results compared to controls. After adjusting for age and sex, post-COVID subjects continued to have a greater change in HR and BP with AS and TT and a lower RSA compared to controls. However, with this adjustment several differences compared to the PAF group were attenuated (Table 3).
Conclusion: Post-COVID subjects were observed to have multiple quantitative autonomic testing abnormalities. Once corrected for sex and age, AD severity in post-COVID-19 patients is comparable to that seen in neurodegenerative PAF.
Objective: Compare autonomic testing measures of post-COVID-19 subjects to controls and those with pure autonomic failure (PAF).
Methods: Autonomic testing included 1) change in heart rate (HR) and blood pressure (BP) with active standing (AS) and tilt table testing (TT), 2) time to BP nadir and recovery during AS and TT, 3) Valsalva ratio (VR), and 4) respiratory sinus arrhythmia (RSA). Comparisons between two groups were made using t-tests, Kruskal-Wallis, or chi-square tests. Multivariable linear regression was used to adjust findings for age and sex. A p-value of <0.05 was considered significant.
Results: Control subjects (n=25, median 32 [21-39] years, 76% female) and post-COVID patients (n=91, median 36 [25-50] years, 84% female, mean 11.96 [±9.14] months from infection) were similar in age and sex, while the PAF group (n=38, median 64 [56-74] years, 53% female) was older and comprised of more males (Table 1). The VR and RSA of the post-COVID group was significantly lower than controls, but higher than the PAF group (Table 2). The change in BP with AS and TT for post-COVID subjects was significantly higher than controls and lower than the PAF group. The post-COVID group also had a significantly increased change in HR with TT compared to both the control and PAF groups. Across all four tests, the post-COVID group had a higher proportion of abnormal results compared to controls. After adjusting for age and sex, post-COVID subjects continued to have a greater change in HR and BP with AS and TT and a lower RSA compared to controls. However, with this adjustment several differences compared to the PAF group were attenuated (Table 3).
Conclusion: Post-COVID subjects were observed to have multiple quantitative autonomic testing abnormalities. Once corrected for sex and age, AD severity in post-COVID-19 patients is comparable to that seen in neurodegenerative PAF.
More abstracts on this topic:
Cardiac-Selective TRPV1 Afferent Ablation in Subacute Myocardial Infarction Ameliorates Adverse Remodeling and Ventricular Arrhythmogenesis
Masuyama Kiyoshi, Ajijola Olujimi, Chung Wei-hsin, Cha Steven, Patel Janaki, Haridas Sahil, Doan Nhi, Abhyankar Devaki, Challita Ronald, Su Maureen
Cardiorenal Dysfunction Caused by High Fat Diet and Sodium Oxalate Gavage in MiceSilva Amanda, Irigoyen Maria, Nascimento-carvalho Bruno, Jimenez Alessandra, Silva Maikon, De Oliveira Silva Tábatha, Lunardon Guilherme, Souza Felipe, Andrade Lucia, Diniz Gabriela