Final ID: MDP1324
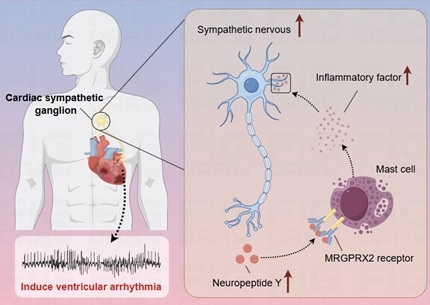
Mast cell MRGPRX2 receptor-mediated neuroimmune interaction induces ventricular arrhythmias after acute myocardial infarction via the overactivation of cardiac sympathetic nerves system
Abstract Body (Do not enter title and authors here): Background: Previous study has shown mast cell (MC) can modulate cardiac sympathetic nerve activity, associated with ventricular arrhythmias after myocardial infarction (MI). However, the key receptor that play a role in this remain unknown.
Hypothesis: MRGPRX2 is a newly identified MC receptor that primarily mediates neuroimmune responses. We hypothesized it plays an important role in ventricular arrhythmias after MI.
Methods: Cardiac sympathetic ganglion tissues and blood were collected from normal, acute MI and chronic MI models for preliminary detection of MRGPRX2 expression. Plasma of acute MI and normal coronary arteries patients was collected for the determination of relevant indices. Knockdown of MRGPRX2 in cardiac sympathetic nerve to explore its role and mechanisms in ventricular arrhythmias after acute MI.
Results: In normal models, expression of MRGPRX2 and FcεRI receptors in cardiac sympathetic nervous were significantly higher than other common MC receptors. We found increased expression of MRGPRX2, corresponding ligand neuropeptide Y (NPY) and MC inflammatory factors in acute MI models. No similar trend was observed for IgE-FcεRI pathway. Clinical data showed serum MRGPRX2 levels were higher in acute MI group than in the control group [1.002 (0.675-1.301) vs. 0.661 (0.562-0.887), P<0.05], and were positively correlated with serum NPY and inflammatory factors levels. In acute MI models, knockdown of MRGPRX2 reduced the sympathetic indexes of heart rate variability and serum NPY, resulting in suppressed cardiac sympathetic activity. And it suppressed local inflammation and sympathetic remodeling. Moreover, it could improve ventricular electrophysiological stability, evidenced by the prolonged ventricular effective refractory period, elevated action potential duration, increased ventricular fibrillation threshold, consequently showing antiarrhythmic effects.
Conclusion: MRGPRX2 receptor-mediated neuroimmune disorders induce ventricular arrhythmias after MI, suggesting that MRGPRX2 is a potential target for therapy.
Hypothesis: MRGPRX2 is a newly identified MC receptor that primarily mediates neuroimmune responses. We hypothesized it plays an important role in ventricular arrhythmias after MI.
Methods: Cardiac sympathetic ganglion tissues and blood were collected from normal, acute MI and chronic MI models for preliminary detection of MRGPRX2 expression. Plasma of acute MI and normal coronary arteries patients was collected for the determination of relevant indices. Knockdown of MRGPRX2 in cardiac sympathetic nerve to explore its role and mechanisms in ventricular arrhythmias after acute MI.
Results: In normal models, expression of MRGPRX2 and FcεRI receptors in cardiac sympathetic nervous were significantly higher than other common MC receptors. We found increased expression of MRGPRX2, corresponding ligand neuropeptide Y (NPY) and MC inflammatory factors in acute MI models. No similar trend was observed for IgE-FcεRI pathway. Clinical data showed serum MRGPRX2 levels were higher in acute MI group than in the control group [1.002 (0.675-1.301) vs. 0.661 (0.562-0.887), P<0.05], and were positively correlated with serum NPY and inflammatory factors levels. In acute MI models, knockdown of MRGPRX2 reduced the sympathetic indexes of heart rate variability and serum NPY, resulting in suppressed cardiac sympathetic activity. And it suppressed local inflammation and sympathetic remodeling. Moreover, it could improve ventricular electrophysiological stability, evidenced by the prolonged ventricular effective refractory period, elevated action potential duration, increased ventricular fibrillation threshold, consequently showing antiarrhythmic effects.
Conclusion: MRGPRX2 receptor-mediated neuroimmune disorders induce ventricular arrhythmias after MI, suggesting that MRGPRX2 is a potential target for therapy.