Final ID: Su4171
The Impact of a Closed Unit Model on Cardiac Intensive Care Unit Outcomes: A Before-After Study
Abstract Body (Do not enter title and authors here): Background: The ‘closed unit model’ is increasingly being adopted as a model for providing critical care to cardiac patients in contemporary intensive care units (ICU), where patients are under the direct care of an intensivist-led primary team. Many data demonstrates improved outcomes in various other intensive care settings, but few data exist in the context of cardiology intensive care. We aim to assess the clinical implications of adopting a closed unit model in our cardiac intensive care unit (CICU) across a variety of parameters.
Hypothesis: Adoption of a closed unit model will result in improvement in mortality rate, ICU length of stay (LOS), and spontaneous awakening trial (SAT) and spontaneous breathing trial (SBT) compliance.
Methods: We performed a before—after retrospective comparison of patients admitted to the CICU at our tertiary care hospital after adoption of a closed unit model on 1 January. The study period was the first 3 months after adoption of the closed model, with the 3-months preceding adoption of the closed model serving as the comparison group. Mortality, SAT and SBT rates were compared using the Chi-squared test and median CICU LOS was compared using the Wilcoxon rank-sum test.
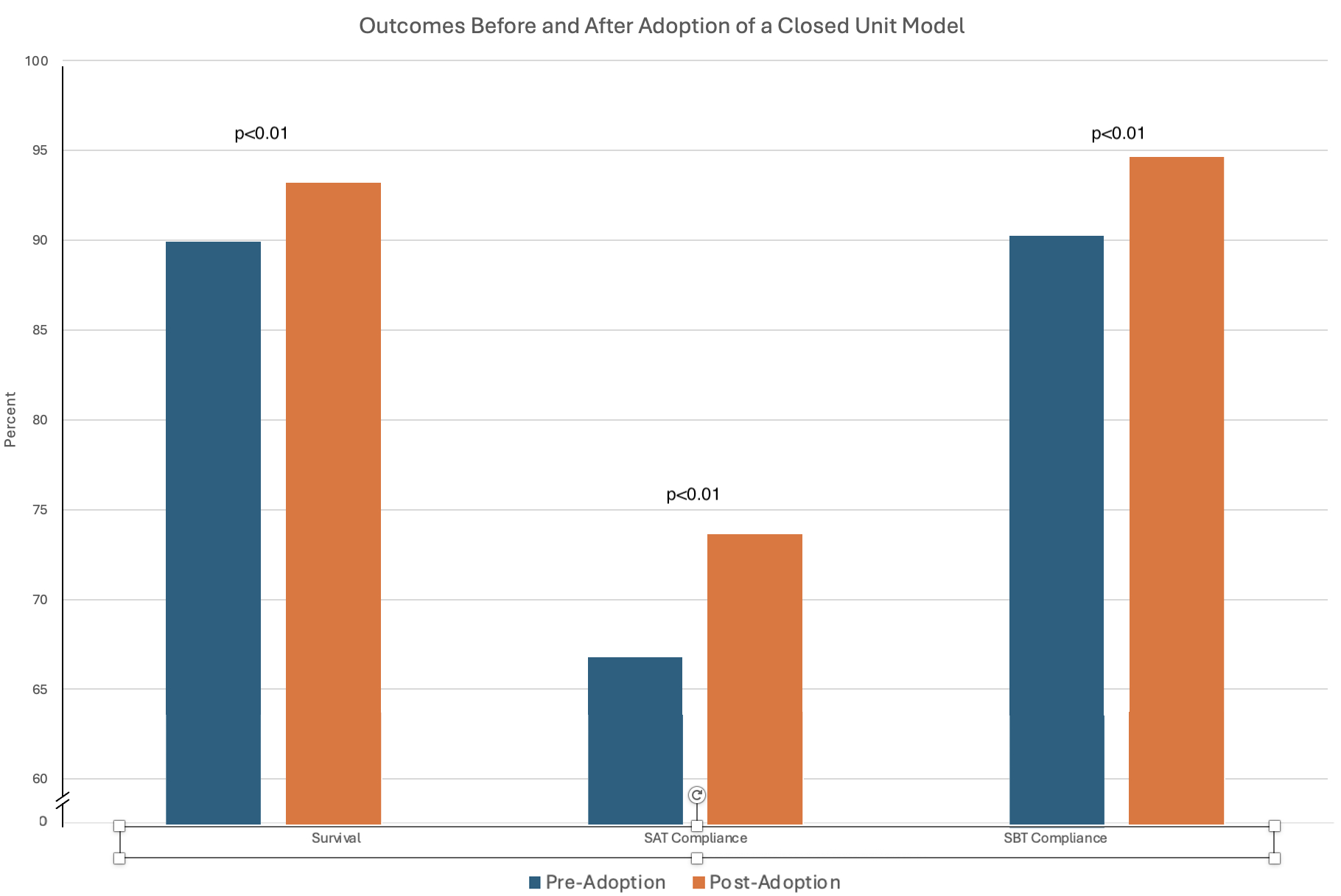
Results: 751 individual patients were admitted to the CICU and analyzed (380 before vs 371 after adoption). The mortality rate significantly improved (10% vs 6.7%; p=<0.01; Figure 1). Despite this, there was no significant change in median LOS (2.7 days [IQR 1.11-5.73] vs 2.5, [IQR 1.16-6.14]; p=0.54). There was also a significant improvement in SAT (66.8% vs. 73.6%; p=<0.01) and SBT rates (90.3% vs. 94.6%; p=<0.01; Figure 1).
Conclusions: Adoption of a closed unit model resulted in a statistically significant improvement in CICU mortality and daily SAT and SBT compliance, although surprisingly there was no improvement in LOS. These findings suggest that our transition to a closed unit model enhanced our patient's outcomes likely through promoting improved adherence to evidence-based critical care principles. Further study is needed to explore the factors contributing to the unchanged LOS and to better evaluate the long-term impact of a closed unit model on outcomes and resource utilization in cardiac ICUs.
Hypothesis: Adoption of a closed unit model will result in improvement in mortality rate, ICU length of stay (LOS), and spontaneous awakening trial (SAT) and spontaneous breathing trial (SBT) compliance.
Methods: We performed a before—after retrospective comparison of patients admitted to the CICU at our tertiary care hospital after adoption of a closed unit model on 1 January. The study period was the first 3 months after adoption of the closed model, with the 3-months preceding adoption of the closed model serving as the comparison group. Mortality, SAT and SBT rates were compared using the Chi-squared test and median CICU LOS was compared using the Wilcoxon rank-sum test.
Results: 751 individual patients were admitted to the CICU and analyzed (380 before vs 371 after adoption). The mortality rate significantly improved (10% vs 6.7%; p=<0.01; Figure 1). Despite this, there was no significant change in median LOS (2.7 days [IQR 1.11-5.73] vs 2.5, [IQR 1.16-6.14]; p=0.54). There was also a significant improvement in SAT (66.8% vs. 73.6%; p=<0.01) and SBT rates (90.3% vs. 94.6%; p=<0.01; Figure 1).
Conclusions: Adoption of a closed unit model resulted in a statistically significant improvement in CICU mortality and daily SAT and SBT compliance, although surprisingly there was no improvement in LOS. These findings suggest that our transition to a closed unit model enhanced our patient's outcomes likely through promoting improved adherence to evidence-based critical care principles. Further study is needed to explore the factors contributing to the unchanged LOS and to better evaluate the long-term impact of a closed unit model on outcomes and resource utilization in cardiac ICUs.
More abstracts on this topic:
Advancing Age, ASA Class, Sex, Functional Status, and Comorbidities as Predictors of Perioperative Cardiac Arrest Following Total Hip Arthroplasty: A National Cohort Study
Hussain Abdur-rehman, Soni Ashesh, Stead Thor, Persaud Nadiya, Ganti Latha
A Stepwise Approach to Identifying and Assessing the Content Validity of Patient-Reported Outcome (PRO) Measures for Use with Adults with Acute Heart FailureO'connor Meaghan, Loughlin Anita, Waldman Laura, Rucker Sloan, Vaghela Shailja, Kwon Namhee, Sikirica Vanja