Final ID: MDP143
Higher t-PA Doses are Associated with Reduced In-Hospital Mortality in Pulmonary Embolism Patients Undergoing Catheter-Directed Thrombolysis
Abstract Body (Do not enter title and authors here): Background: Pulmonary embolism (PE) is a leading cause of cardiovascular death and preventable hospital mortality in the US. High-risk acute PE has a 30% mortality rate, despite new treatments like catheter-directed thrombolytics (CDT). CDT has shown to improve right ventricle/left ventricle (RV/LV) diameter ratio compared to anticoagulation alone, but the optimal t-PA dose is uncertain. Traditional dosing is 10-24 mg over 12-24 hours, but clinical trials have showed similar RV/LV diameter ratio reductions with lower doses and shorter infusions. No prospective data has shown a mortality benefit.
Hypothesis: Higher t-PA doses will improve in-hospital mortality, length of stay (LOS), pulmonary artery (PA) pressure reduction, and cardiac biomarker reduction in patients receiving CDT for acute PE.
Methods: We retrospectively analyzed patients who presented with PE and underwent CDT at a single center, tertiary hospital. Patients were stratified by t-PA dose (<24mg vs ≥24mg). Outcomes were compared using adjusted linear or logistic regression models.
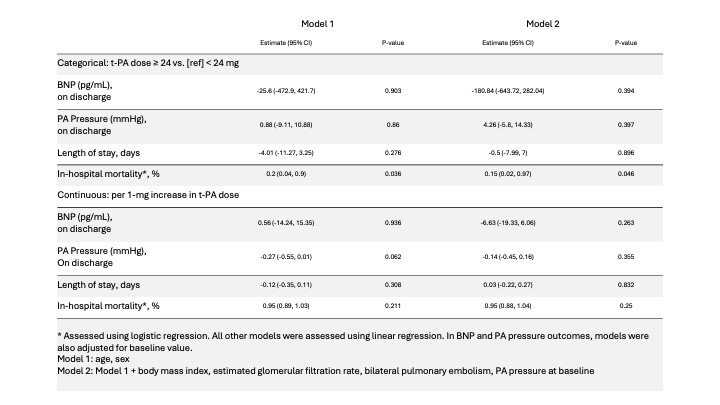
Results: Among 133 patients, 105 (80%) received t-PA ≥24mg. Patients who received higher doses of t-PA were younger (61 vs. 71 years, p=0.02), more likely to have bilateral PE (93% vs 77%; p=0.03) and had higher BMI (35 vs 30.5; p=0.04) and PA pressure (51 vs 40.5 mmHg; p=0.003) at baseline. In unadjusted analysis, no significant difference in in-hospital mortality was observed with t-PA ≥24mg (3.8% vs. 16.4%, p=0.08). However, in the adjusted analysis, a significantly lower risk in-hospital mortality rate was observed with t-PA ≥ 24mg (OR 0.15, 95%CI 0.02-0.97, p=0.046) (Table). No significant differences were observed in BNP reduction, PA pressure change, or LOS (Table).
Conclusion: In acute PE patients undergoing CDT, t-PA dosing ≥24mg was associated with reduced in-hospital mortality. Prospective randomized controlled trials are needed to further define optimal dosing protocols.
Hypothesis: Higher t-PA doses will improve in-hospital mortality, length of stay (LOS), pulmonary artery (PA) pressure reduction, and cardiac biomarker reduction in patients receiving CDT for acute PE.
Methods: We retrospectively analyzed patients who presented with PE and underwent CDT at a single center, tertiary hospital. Patients were stratified by t-PA dose (<24mg vs ≥24mg). Outcomes were compared using adjusted linear or logistic regression models.
Results: Among 133 patients, 105 (80%) received t-PA ≥24mg. Patients who received higher doses of t-PA were younger (61 vs. 71 years, p=0.02), more likely to have bilateral PE (93% vs 77%; p=0.03) and had higher BMI (35 vs 30.5; p=0.04) and PA pressure (51 vs 40.5 mmHg; p=0.003) at baseline. In unadjusted analysis, no significant difference in in-hospital mortality was observed with t-PA ≥24mg (3.8% vs. 16.4%, p=0.08). However, in the adjusted analysis, a significantly lower risk in-hospital mortality rate was observed with t-PA ≥ 24mg (OR 0.15, 95%CI 0.02-0.97, p=0.046) (Table). No significant differences were observed in BNP reduction, PA pressure change, or LOS (Table).
Conclusion: In acute PE patients undergoing CDT, t-PA dosing ≥24mg was associated with reduced in-hospital mortality. Prospective randomized controlled trials are needed to further define optimal dosing protocols.
More abstracts on this topic:
Acute Right Ventricular Systolic Dysfunction Diagnosed by Transesophageal Echocardiography in Patients Post-Cardiac Arrest and Undifferentiated Shock: The Role of Clot in Transit Detection
Dieiev Vladyslav, Salinas Pedro
Accelerating Stroke Care at an Academic Hospital: Evaluating the Impact of a Launchpad Initiative on Door-to-Needle Times One Year LaterShoemaker Camella, Shugrue Leah, Coccia Michael, Bakradze Ekaterina, Shapshak Dag, Gropen Toby, Thompson Karen, Taylor Danielle, Morrison Amanda, Stallings Ashley, Shipley Sarah, Jones Tamicka, Rafferty Rachael, Reid Tonya