Final ID: Su4111
Ischemic Stroke and TIA Incidence in Transcatheter Aortic Valve Replacement Versus Surgical Aortic Valve Replacement: A Comparative Systematic Review and Meta-analysis
Abstract Body (Do not enter title and authors here): Objective: This systematic review and meta-analysis aimed to compare the incidence of ischemic stroke and Transient ischemic attack (TIA) post-transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR) in intermediate or high surgical risk patients with aortic stenosis, as this assessment may influence the choice of intervention.
Methods: In accordance with PRISMA guidelines, we conducted a comprehensive search of PubMed, Google Scholar, and Cochrane CENTRAL databases from inception to December 2023 to identify trials and observational studies comparing the incidence of stroke and TIA after 30 days and 1-year post-TAVR vs SAVR from their inception through December 2023. Odds ratios (ORs) with 95% confidence intervals (CIs) for each study, employing a random-effects model for data synthesis irrespective of heterogeneity, were utilized as measures of outcomes. Heterogeneity was assessed using I2 statistics. All statistical analyses were conducted using Review Manager (Rev Man, Version 5.4; The Cochrane Collaboration, Copenhagen, Denmark).
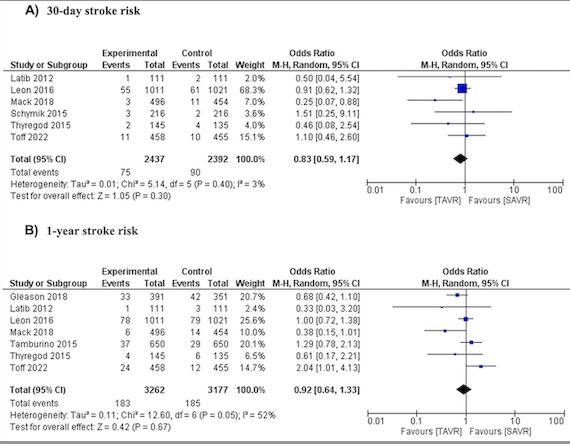
Results: After screening of 4549 articles, eight randomized controlled trial studies consisting of 5 randomized controlled trials and three observational studies with a total of 6879 patients were included in this meta-analysis; six studies comparing 30-day stroke incidence, no significant difference was found between TAVR and SAVR (OR 0.83, 95% CI 0.59 to 1.17, p=0.30, I2 3%). Seven studies showed that TAVR patients had a similar 1-year stroke risk to SAVR patients (OR 0.92, 95% CI 0.64 to 1.33, p=0.67, I2 52%). In the TIA case, there was no evidence of a significant difference between TAVR and SAVR in the risk of having a transient ischemic attack within 30 days following surgery (OR 0.93, 95% CI 0.24 to 3.63, p=0.92, I2 52%), although There was a greater 1-year risk of having a transient ischemic attack in the TAVR group compared to the SAVR group, OR 1.15 (95% CI 0.72 to 1.82, p=0.56, I2 0%), however, this was not a statistically significant difference.
Conclusion: Our meta-analysis showed no significant differences in either ischemic stroke or TIA occurrences within 30 days and 1-year post TAVR and post SAVR in intermediate or high surgical risk patients.
Methods: In accordance with PRISMA guidelines, we conducted a comprehensive search of PubMed, Google Scholar, and Cochrane CENTRAL databases from inception to December 2023 to identify trials and observational studies comparing the incidence of stroke and TIA after 30 days and 1-year post-TAVR vs SAVR from their inception through December 2023. Odds ratios (ORs) with 95% confidence intervals (CIs) for each study, employing a random-effects model for data synthesis irrespective of heterogeneity, were utilized as measures of outcomes. Heterogeneity was assessed using I2 statistics. All statistical analyses were conducted using Review Manager (Rev Man, Version 5.4; The Cochrane Collaboration, Copenhagen, Denmark).
Results: After screening of 4549 articles, eight randomized controlled trial studies consisting of 5 randomized controlled trials and three observational studies with a total of 6879 patients were included in this meta-analysis; six studies comparing 30-day stroke incidence, no significant difference was found between TAVR and SAVR (OR 0.83, 95% CI 0.59 to 1.17, p=0.30, I2 3%). Seven studies showed that TAVR patients had a similar 1-year stroke risk to SAVR patients (OR 0.92, 95% CI 0.64 to 1.33, p=0.67, I2 52%). In the TIA case, there was no evidence of a significant difference between TAVR and SAVR in the risk of having a transient ischemic attack within 30 days following surgery (OR 0.93, 95% CI 0.24 to 3.63, p=0.92, I2 52%), although There was a greater 1-year risk of having a transient ischemic attack in the TAVR group compared to the SAVR group, OR 1.15 (95% CI 0.72 to 1.82, p=0.56, I2 0%), however, this was not a statistically significant difference.
Conclusion: Our meta-analysis showed no significant differences in either ischemic stroke or TIA occurrences within 30 days and 1-year post TAVR and post SAVR in intermediate or high surgical risk patients.
More abstracts on this topic:
A Multi-centre, Randomized, Controlled Study of External CounterPulsation for Patients with Recent Atherosclerotic Stroke (SPA)
Xiong Li, Chen Xiangyan, Leung Howan, Zhu Lixia, Leung Thomas, Wong Lawrence
A Meta-Analysis of Prospective Studies Comparing Short and Longterm Outcomes of Trans-Catheter Aortic Valve Replacement in Patient with and without Cancer:Khan Muhammad Aslam, Haider Adnan, Haider Taimoor, Bhattarai Shraddha, Khan Bilal, Lamichhane Bikal, Shafique Nouman, Rahman Hammad, Aafreen Asna, Muhammad Anza, Bhatia Hitesh, Khan Abid Nawaz Khan, Akbar Usman, Khan Alamzaib