Final ID: Su2022
Single Ventricle Palliation Pathways: Patient Characteristics and Outcomes
Abstract Body (Do not enter title and authors here): Introduction
The choice between conventional surgical (SP) and hybrid (HP) stage 1 palliation for single ventricle heart disease remains debated. Pulmonary artery banding and prostaglandins followed by delayed surgical stage 1 (DSP) remains another option. HP is proposed for high-risk patients. We aimed to describe index hospitalization outcomes for patients undergoing these 3 pathways. We hypothesized that patients undergoing HP and DSP have more comorbid conditions, higher morbidity, and longer length of stay (LOS).
Methods
Using the Pediatric Health Information System data, January 2016 – August 2023, we analyzed the characteristics and index hospitalization outcomes for patients with single ventricle disease undergoing SP, HP, and DSP.
Results
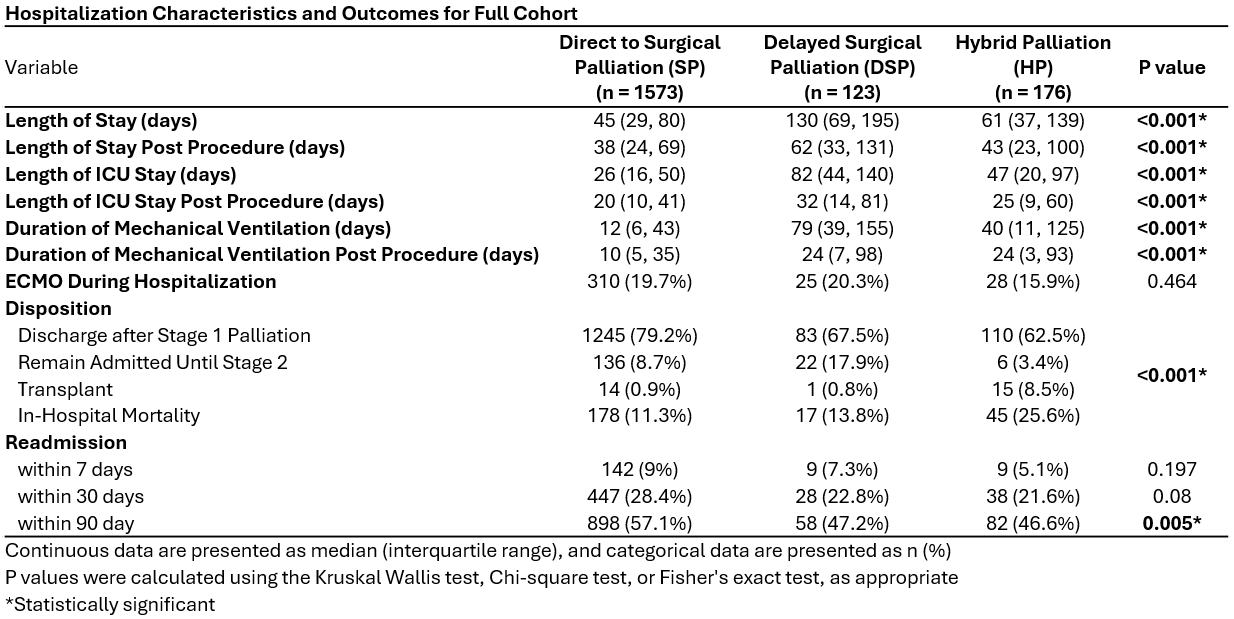
Our final cohort included 1,872 patients (1,573 SP; 176 HP; 123 DSP). Prematurity was most common (45.5%) in the DSP compared to the HP (27.8%) and SP (9.5%) groups (P<0.001); the rate of small for gestational age birth (SGA, <2.5 kg) was similarly distributed. Non-cardiac comorbidities were most prevalent in DSP (neurologic, gastrointestinal, need home technology) and HP (respiratory). LOS (days) was highest for DSP (median 130, IQR:69–195) compared to HP (median 61, IQR:37–139) and SP (median 45, IQR:29–80)(P<0.001). Disposition varied (P<0.001), with in-hospital mortality highest among HP (25.6%) compared to DSP (13.8%) and SP (11.3%); the rate of index hospitalization heart transplant was 8.5% for HP, DSP 0.8%, and SP 0.9%.
Among patients born prematurely or SGA, LOS was longest for DSP (median 143, IQR:88–216) followed by HP (median 72, IQR:52–139) and SP (median 59, IQR:36–124)(P<0.001). Disposition also varied (P=0.004), with higher in-hospital mortality among HP (35.9%) compared to DSP (16.9%) and SP (19.9%); transplant was highest among HP (4.7%) compared to DSP (0%) and SP (0.8%).
Adjusted total costs per hospital day did not vary significantly.
Conclusions
Patients undergoing DSP and HP are more often premature or SGA. Patients undergoing HP are most likely to have index hospitalization mortality or transplant. While recognizing the limitations of administrative databases, our data does describe the current utilization trend and outcomes for SP, HP, and DSP.
The choice between conventional surgical (SP) and hybrid (HP) stage 1 palliation for single ventricle heart disease remains debated. Pulmonary artery banding and prostaglandins followed by delayed surgical stage 1 (DSP) remains another option. HP is proposed for high-risk patients. We aimed to describe index hospitalization outcomes for patients undergoing these 3 pathways. We hypothesized that patients undergoing HP and DSP have more comorbid conditions, higher morbidity, and longer length of stay (LOS).
Methods
Using the Pediatric Health Information System data, January 2016 – August 2023, we analyzed the characteristics and index hospitalization outcomes for patients with single ventricle disease undergoing SP, HP, and DSP.
Results
Our final cohort included 1,872 patients (1,573 SP; 176 HP; 123 DSP). Prematurity was most common (45.5%) in the DSP compared to the HP (27.8%) and SP (9.5%) groups (P<0.001); the rate of small for gestational age birth (SGA, <2.5 kg) was similarly distributed. Non-cardiac comorbidities were most prevalent in DSP (neurologic, gastrointestinal, need home technology) and HP (respiratory). LOS (days) was highest for DSP (median 130, IQR:69–195) compared to HP (median 61, IQR:37–139) and SP (median 45, IQR:29–80)(P<0.001). Disposition varied (P<0.001), with in-hospital mortality highest among HP (25.6%) compared to DSP (13.8%) and SP (11.3%); the rate of index hospitalization heart transplant was 8.5% for HP, DSP 0.8%, and SP 0.9%.
Among patients born prematurely or SGA, LOS was longest for DSP (median 143, IQR:88–216) followed by HP (median 72, IQR:52–139) and SP (median 59, IQR:36–124)(P<0.001). Disposition also varied (P=0.004), with higher in-hospital mortality among HP (35.9%) compared to DSP (16.9%) and SP (19.9%); transplant was highest among HP (4.7%) compared to DSP (0%) and SP (0.8%).
Adjusted total costs per hospital day did not vary significantly.
Conclusions
Patients undergoing DSP and HP are more often premature or SGA. Patients undergoing HP are most likely to have index hospitalization mortality or transplant. While recognizing the limitations of administrative databases, our data does describe the current utilization trend and outcomes for SP, HP, and DSP.
More abstracts on this topic:
A Royal Flush: A Unique Case of Carcinoid Heart Disease Manifesting in a Rare Fashion as Quadruple Valve Involvement
Fraser Elise, Rodriguez L, Mehta Anand, Unai Shinya, Alencherry Ben
Altered Cardiac Cell Populations in Hypoplastic Left Heart SyndromeMorton Sarah, Seidman Christine, Brown Kemar, Wei Eric, Gorham Joshua, Mcdonough Barbara, Beyer Martin, Neyazi Meraj, Layton Olivia, Seidman Jonathan